L1 Training Manual

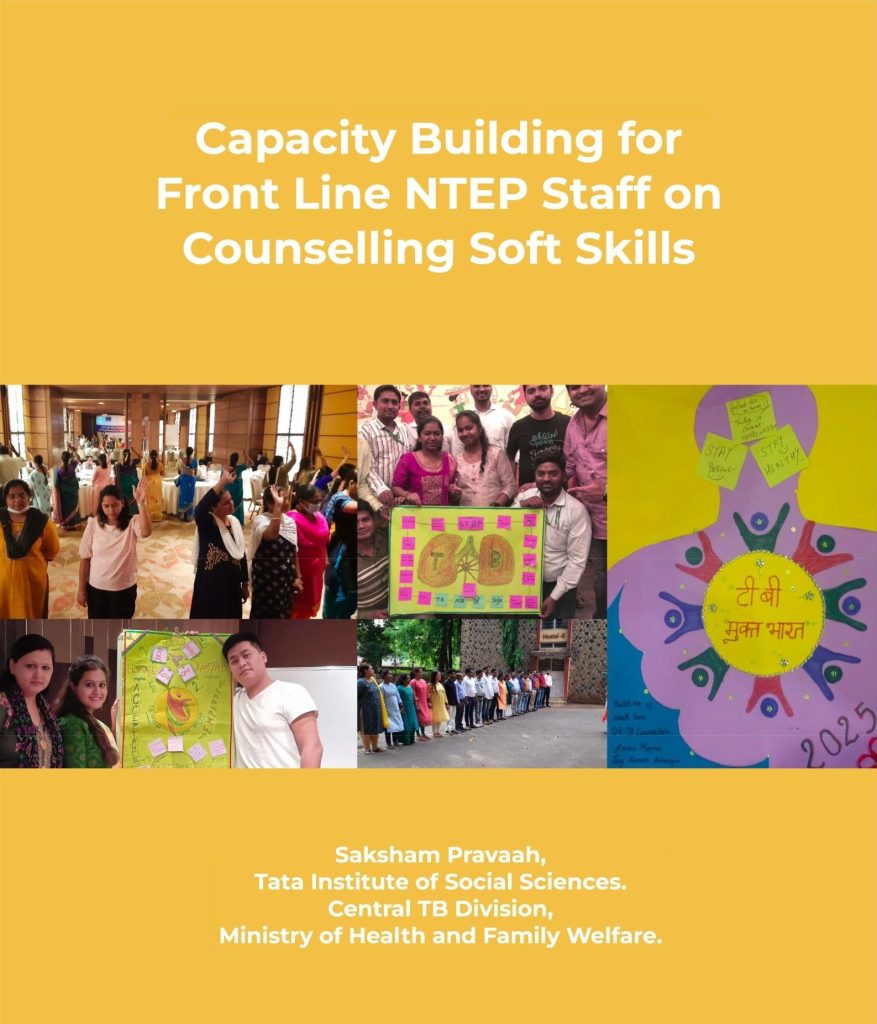
Capacity Building for Front Line NTEP Staff on Counselling Soft Skills
Level – 1
Saksham Pravaah,
Tata Institute of Social Sciences.
Central TB Division,
Ministry of Health and Family Welfare.
This manual is a culmination of the experiences of Saksham (2008-2015), Saksham Prerak (2018- 2020) and Saksham Pravach (2015 onward). The project was funded by Global Fund since 2008 to support the Ministry of Health and Family Welfare in its fight against HIV and TB. Saksham alone is responsible for the views expressed in this manual and permission is required to reproduce any part of this manual, partly or in entirety.
Suggested citation:
‘Capacity Building for Front Line NTEP Staff on Counselling Soft Skills’
Level – 1
Saksham Pravaah, Tata Institute of Social Sciences, Deonar, Mumbai-400088 Central TB Division, Ministry of Health and Family Welfare, Government of India
Published and disseminated by: Saksham Pravaah,
Tata Institute of Social Sciences,
V. N. Purav Marg, Deonar,
Mumbai-400088, India
Office: 91-22-25525491
Email: saksham@tiss.edu
Website: www.tiss.edu
Messages
Contents
| Sr. No. | Title |
|---|---|
| 1 | List of Abbreviations |
| 2 | Background of Saksham |
| 3 | Introduction to the Manual |
| 4 | Checklists for tasks Before/During/After the Training |
| 5 | Training Agenda |
| 6 | Pre and Post Training Evaluation Form |
| 7 | S1: Introductory Session: Who are We and Our Aspirations! |
| 8 | S2: Understanding Social Determinants of TB |
| 9 | S3: Understanding Social Protection Linkages |
| 10 | S4: Introduction to Counselling and Principles of Counselling |
| 11 | S5: Stages and Process of Counselling |
| 12 | S6: Counselling Micro-skills |
| 13 | S7: Enhancing Counselling Competencies for TB |
| 14 | S8: Critical Issues in Adherence Counselling |
| 15 | S9: Our words… Our Perspectives |
| 16 | Hamare Shabd … Hamara Nazariya |
| 17 | Going Ahead… Hum Hain Saksham |
| 18 | Energisers |
List of Abbreviations
| ACF | Active TB Case Finding |
| ADR | Adverse Drug Reaction |
| AIC | Airborne Infection Control |
| ANM | Auxiliary Nurse Midwife |
| AIDS | Acquired lmmuno Deficiency Syndrome |
| ANC | Antenatal Care |
| CBC | Capacity Building Coordinator |
| CBS | Capacity Building Specialist |
| CDO | Chief Development Officer |
| CP | Continuation Phase |
| CTD | Central TB Division |
| CSR | Corporate Social Responsibility |
| DBT | Direct Benefit Transfer |
| DOTS | Directly Observed Treatment Short-course |
| DR-TB | Drug Resistant Tuberculosis |
| DS-TB | Drug Sensitive Tuberculosis |
| DTC | District TBCentre |
| DTO | District Tuberculosis Officer |
| FG | Facilitators’ Guide |
| HCW | Health Care Worker |
| HIV | Human lmmuno Deficiency Virus |
| IP | Intensive Phase |
| IUD | Intrauterine Device |
| KAS | Knowledge, Attitudes and Skills |
| LFU | Loss to Follow Up |
| LWS | Link Workers Schemes |
| MDR-TB | Multi Drug Resistant TB |
| MT | Master Trainer |
| NACP | National AIDS Control Programme |
| NGO | Non-Governmental Organization |
| NTEP | National TB Elimination Programme |
| NSP | National Strategic Plan |
| PPT | PowerPoint Presentation |
| PLHIV | People Living with HIV |
| PHC | Primary Health Centre |
| RTI | Reproductive Tract Infection |
| STDC | State TB Training and Demonstration Centre |
| STI | Sexually Transmitted Infection |
| TB | Tuberculosis |
| TG | Transgender |
| TI | Targeted Intervention |
| TISS | Tata Institute of Social Sciences |
| TPT | Tuberculosis Preventive Treatment |
| WHO | World Health Organization |
Background of Saksham
Background of Saksham

Saksham (which means “making capable”) is a project of the Tata Institute of Social Sciences, funded by the Global Fund since 2008, to support the Ministry of Health and Family Welfare in its fight against HIV and TB. The Saksham project focuses on supporting and strengthening national response for both HIV and TB. Saksham, in partnership with the National AIDS Control Programme (NACP), has developed the curriculum for HIV Counsellors across India and has partnered with the National TB Elimination Programme (NTEP) to provide counselling and psycho-social support for People Living with Drug Resistant TB in Maharashtra, Gujarat, Karnataka and Rajasthan. Currently Saksham has three major grants in the areas of TB counselling, community engagement and HIV evaluations.
Saksham Prerak was HIV response vertical of Saksham. The Project focused on strengthening human resources for health under NACP as well as its integration into National Health Mission through HR- task sharing/task shifting. By the end of the project implementation on March 31, 2021, a total of 13,638 ANMs from 8,193 facilities were trained in HIV and Syphilis screening, while 7,434 HIV Counsellors underwent training to enhance their skills and attitudes.
Saksham Prerak has also developed an e-module for virtual training on clinical aspects of HIV/AIDS. The process of integrating the module with the NIC (National Informatics Centre) server is underway. Saksham has been awarded a project by the NACO for undertaking programmatic as well as Targeted Intervention (Tl) and Link Workers Schemes (LWS) evaluation under NACP across India. The project is named “Saksham Pramaan” and the project duration is April l, 2021 to March31, 2024. Under this project approximately 1600 Tl/ LWS will be evaluated and three major and nine minor programmatic evaluation research studies will be conducted.
Saksham Pravaah is TB vertical of Saksham that introduced psycho-social counselling for TB in Maharashtra, Gujarat, Karnataka, Rajasthan and has demonstrated the need for addressing social determinants of TB. The project is named “Saksham Pravaah” and 214 Professional Counsellors (Master’s in Social Work/ Sociology/ Psychology) are integrated within the NTEP. From programme initiation in October 2015 until March 2021, Saksham Pravaah has provided counselling and psycho-social support to over 80,000 People living with Drug Resistant (DR) TB and their caregivers. The Counsellors provide ongoing home based counselling and address a range of issues including TB related stigma and discrimination, gender-based concerns and mental health. In order to reduce the catastrophic burden of TB, the Counsellors link people living with TB to the available Government of India Social Protection Scheme and Nutrition Support. In the third phase of implementation (April 2021 – March 2024), Saksham Pravaah will create a pool of National Master Trainers to build capacities of front line TB staff on counselling soft skills.
Saksham, in collaboration with the Mumbai District TB Control Society, undertook an initiative to engage TB Survivors meaningfully and gainfully under Saksham Jan Urja project. The project is funded by Tata Power Development Trust and was initiated in January 2020. The Survivors are termed “Saksham (Against TB) Saathi” and undertake telephone counselling to address stigma, present a positive picture of TB treatment, debunk myths around TB and emphasise importance of treatment adherence. The model was integrated within the NTEP from November 2021 in Mumbai and 24 Saksham Saathis were placed within the TB Centres in Mumbai.
Please visit www.tiss.edu (Initiatives/ Saksham) and follow us on
YouTube: https://www.youtube.com/channel/UC3lSzS3nvEAs1MMH0s-Xo2A
Facebook: https://www.facebook.com/sakshamtiss
Twitter: https://www.instagram.com/saksham_tiss/
lnstagram: https://twitter.com/SakshamTiss
using the links for regular updates about Saksham
Introduction to the Manual
A note for State TB Training and Demonstration Centres
(STDC) and Master Trainers for using this Manual
This manual is prepared based on the HIV Counselling Training Experience and implementing DRTB Counselling services of Saksham, TISS. The manual is intended for the training of front line NTEP staff who are new to the concept of Counselling. These concepts have been broken down and simplified for ease of understanding.
The training manual is aimed at providing the front line NTEP Staff with an opportunity to understand the principles of Counselling, practice the skills of Counselling and linkages for social protection schemes in a participatory and experiential manner.
The manual provides a basic outline of the activities that include statements, case scenarios and case studies. Please feel free to change them to local/regional context. Please translate all the case studies/statements in the local language before taking the session. Links for Hindi translation of Annexures/ Handouts for further readings are included in the manual after every session.
The training curriculum outlined through this manual is not aimed to be exhaustive for TB related care, but focuses on training Counselling Skills to the NTEP staff. The instructions here are meant for the State TB Training and Demonstration Centre (STDC)/ Master Trainers under Saksham Pravaah project of Tata Institute of Social Sciences (TISS) however, it can also be used by any other agency for the training of NTEP staff with suitable modifications.
The training manual consists of 10 sessions. Each session has clearly stated objectives and session plans. The training manual includes two parts which are as follows:
- Facilitator’s Guide (FG), which provides the session plan and an overview of the training content.
- Annexures/ Handouts for further reading and Links for the Hindi translation of the same.
The manual is planned in such a manner that the concepts get built as the training progresses. Ideally, the entire training should be conducted by a team of two or three resource persons who anchor the training and are aware of the training sessions. The resource persons have to keep identifying the links e.g., principles which need to be reflected upon in all sessions. However, in case having two resource persons is not possible, STDC should ensure that the same resource person conducts session 6 – Micro skills and Session 7 – Counselling Competencies, as both sessions are linked.
As a principle, Saksham refers TB Patients as ‘People Living with TB / People living with DR – TB’. However, for the purpose of this manual and for common understanding, term ‘TB Patient’ has been used. For gender inclusiveness Saksham uses the pronoun ‘They’ which includes Women, Men and Transgenders.
- Setting the Stage for Training
No training is complete without the necessary preparations, even if the best training manual and resources are available. The preparations have to set the stage for learning and for achieving the training objectives.
These include:
· Adult learning styles / Participatory training must be planned to ensure involvement of all participants. Learning through discussions, role-plays, brainstorming sessions and games help increase the participants’ receptivity and learning potential. It also helps the Facilitator to understand the level of knowledge and experience of the participants.
· As far as possible, Local language and terminologies should be used during the training in settings where participants are more conversant with the local language. To make the best use of time during the training and to enhance learning, it is advised that the training coordinators get all the training material translated in the local language.
· An introduction and a conclusion for every topic helps the participants recapitulate the main messages from the manual. Key messages are added at the end of every session. The Facilitator needs to ensure that the participants understand and retain these hence, they need to be emphasised.
· Translate the necessary training material. Training schedule and pre & post assessment questionnaires, which are going to be used by the participants, need to be translated in the local language. This will save time and the learning can be significantly enhanced if the language is easily understood by the participants.
Saksham will develop a pool of Master Trainers. The Master Trainers trained according to this manual will be available at the state level for conducting the three-day training for front line staff on counselling soft skills. Although the sessions have been designed to address all aspects of the training, the ultimate success of the training lies with the Facilitators.
The Capacity Building Coordinators (CBCs) will coordinate with the STDC and help in implementing the training programmes for the NTEP front line staff. Coordination includes assigning the manuals to Master Trainers with appropriate experience and assuring that the Master Trainers familiarise themselves with handouts, activities and presentations well before the training.
The Capacity Building Coordinators must send the relevant sections of the manual to Master Trainers who will be the Facilitators, well in advance. The Facilitators need to be asked to follow the session plan and not carry out a session just on one’s own. The activities given in the sessions are of utmost importance. The Capacity Building Coordinators must make sure to carry out these activities as per the session plans to enhance learning and not follow merely a lecture method. - Training Schedule
· The complete set of activities in the manual covers a three-day programme.
· To fit in the very tight schedule of the training, the training has been made residential even for the local participants.
· It is suggested that the training coordinators insist that all the participants reach the training venue a day prior to the first day of the training, so that there are no chances of any participant missing any session due to delays in travel.
· The training needs to start at 9.30 am and go on till around 5.30 pm so that the curriculum can be covered
within the stipulated time.
· Participants need to be requested to return from the breaks (lunch, tea) and settle down well before the start of the next session, for optimal use of time.
· The participants’ return journey needs to be planned on the third day after the training is over, or after 5 pm at the earliest. This will ensure completion of the post-training assessment, evaluation and other formalities which take place after the full day’s training on the third day is over. - Key Considerations for Training
· A good training programme is supposed to equip NTEP staff with communication skills needed while interacting with TB Patient.
· There is also a need to develop attitudes that facilitate such interaction.
· Learning objectives in these areas can be achieved only when the learning methods are interactive
and involve practicing of communication skills and expression of feelings by the participants.
· Training for NTEP staff should be competency-based, bearing in mind the realities of the situation in the field.
The most important method of training in any situation depends on the nature of the learning objectives. For example, the learning of facts requires. different learning methods from the learning of skills. Hence, even though the participants and the Facilitators may be most familiar with the lecture method , this method alone is NOT enough to learn communication skills or counselling skills
3.1 Group size
The group size for the NTEP staff training should not exceed 30-35 participants. The ideal batch size would be about 30.
3.2 Interactive training strategies
This manual uses interactive training methodologies, allowing instructions, practice and feedback to take place. Each session of the training involves one or more of the following strategies:
Role-play exercises
Group discussions
Educational games
Case-based small group learning activities
Brainstorming sessions
Presentations
A PowerPoint (PPT) presentation should be avoided wherever possible. Instead, the key points can be written on the board while facilitating the session. Facilitators need to promote interaction during and in addition to PPT presentations (if any) by:
Explaining in one’s own words rather than reading out the slide word-by-word.
Encouraging questions from the group following the presentation
Conducting group work to discuss and answer questions
Assigning issues or tasks to small groups
Not more than l minute per slide
Visual aids
Visual aids can be used to highlight oral presentations or points. For example, key points can be noted on the blackboard/whiteboard and questions for debate or discussion (and responses) can be written on the board. The use of the board in this way promotes discussions and interactions. Visual aids should be clear and readable and should not be filled with too many details.
Role-plays
Role-plays need to be used to ‘act out’ specific roles of identified people or to act out a scene. This is useful while practicing skills such as counselling and to explore how people react to specific situations. Please refer to the note on guidelines for performing role plays at the end of this section.
Group discussions-large group discussions
Group discussions may be carried out in a large group (involving all the participants) or in smaller groups of 3-4 participants each. Please refer to the note for guidelines on group discussions at the end of this section.
Case studies
Case studies are designed to enable NTEP staff to deal with TB Patients. The Facilitator may need to translate case studies into the local language. Case studies are introduced in the Facilitator Guide which are followed by a discussion of key points pertaining to the case study. Case studies should be printed and provided to the participants as part of the activity. These case studies provide a detailed description of an event, different characters and settings. The case studies may be followed by a series of questions that will challenge the participants to discuss the positive and negative aspects of the event.
The advantages of case studies are that they allow an examination of a problem and help the Facilitators build participants’ confidence and problem-solving skills in their settings. - Use of Master Trainers/Facilitators
Follow these guidelines to maximize the use of Master Trainers or Facilitators:
· Ensure that the Master Trainers are adequately briefed: The Master trainers need to be briefed, both verbally as well as in writing, about what is expected of them. They need to be provided with a guideline that specifies the content to be covered, the methodology to be used, the level and type of language and the time frame. In addition, they need to be clearly explained about the type of participants present in the training and the overall aims of the training programme. Master Trainers need to reach half an hour early so that they can be briefed clearly about these details. Do insist that the time frame is followed under all circumstances, so that the sessions do not keep spilling over into each other.
· While inviting a Master Trainer who has conducted a session earlier, ask them to go through the entire session as the sessions might have undergone some modifications. The Master Trainers should not assume that they know what the
session content.
· Choose Master Trainers who are known to be effective for your goals. Alternatively, ‘groom’ them to attain the desired outcome. - Assessing Participants’ Knowledge Levels
Before beginning the training, assess the participant’s knowledge, attitudes and practices regarding TB with Pre-Training Assessment Tool.
The information gathered through the tool can be used to fine-tune the training to the knowledge level of the participants. At the end of the training, the same assessment tool can be administered to determine how much knowledge and skills have been gained by the participants and how effective the training has been. - Key Considerations for Successful Training
- Ensure that the material required for each session has been made available well in advance.
- Encourage all participants to be present for the ENTIRE training.
- Ensure that the training sessions commence on time. Request all participants to stay at the venue, as it is a residential training even for the local participants. Those who insist on going home, must arrive on time and leave only after all the evening activities are completed. Inform them that there is a considerable amount of material to be covered each day and that it can be very disruptive to have participants arrive late or leave early at the training sessions.
- The organising team members need to be constantly present during the training sessions and be ready with an ample number of energisers to keep the participants interested and alert during the training.
- Encourage participants to ask questions during the session. If the question is not relevant to the topic of the session, it can be answered separately, in person during lunch break or tea break.
- Encourage participants to maintain confidentiality by not disclosing Patient’s identity while sharing their experiences.
- Encourage participants to respect individual differences. Many a times Participants come from different ethnic and cultural groups; and their lifestyles, beliefs, personal experiences and expertise may differ from each other.
- Encourage participants to listen carefully and with empathy and respect each other’s contributions, opinions and experiences. Explain that it is important in the training and as professionals to practice active listening by allowing each other to share their own experiences and opinions with the group.
- Create a congenial environment in which each participant feels comfortable asking questions. Participants need to be able to ask questions about what they do not understand.
- Due to the constant change in treatment, perceptions, attitudes and so on, participants should be reminded to regularly update their information regarding TB.
- Ensure that you get the right participants. Establish clear criteria for participation and communicate these criteria not only to the participants but also to their employers.
Guidelines for Role Plays
Role plays can serve the important purpose of helping the participants practise skills in a safe environment, where no harm can be caused to a ‘real’ Patient and the presence of the Facilitator can provide an opportunity to hone one’s skills. However, role plays may sometimes be seen as a way of practising one’s acting skills which might lead to losing a lot of precious time and also take away from the primary purpose of the training. Thus, the Capacity Building Coordinators as well as Facilitators need to guide role plays well.
The time limit for a role-play needs to be announced before the activity and must be adhered to. The Facilitator needs to emphasise that the focus is on what a Counsellor is doing or saying in the role play and not on the ‘Patient’s’ acting. The group observers need to observe and give feedback on the information provided.
Role-plays have the following advantages:
- They allow for safe rehearsal of skills, activities and information to be shared and provide practical preparation for real world.
- The participants have an opportunity to experience activities and relate theory to practice.
- They allow for full expression and interpretation of concepts.
Some individuals may feel intimidated by role-playing. The Facilitators must be skillful to ensure that they are relaxed and should:- Tell the participants that we all are bound to make mistakes while learning counselling. It is better to make mistakes here rather than in real settings, because here no one is harmed, whereas in the real setting the Patient may get harmed by our mistakes.
- Keep the role-play appropriate to the learning context.
- Always begin by giving positive feedback and then constructively suggest what could have been done additionally or differently.
Guidelines on Group Discussions
Group Discussions-large group discussions
These should be led by the Facilitator and involve the entire group. The advantages of such discussions can be the following:
- The participants are involved in problem-solving.
- The participants are active, which stimulates interest.
- The learning process becomes more personal, requiring the Facilitator to provide feedback on individual opinions and ideas.
- The Facilitator is able to evaluate the participants’ understanding and absorption of the material.
- The participants have an opportunity to share their acquired expertise and skills and learn from each other.
Large group discussions require a skilful Facilitator who: - Asks questions or suggests topics, maintains objectivity and directs the discussion to keep it relevant to the learning objectives.
- Stresses confidentiality.
- Ensures that all group members have an equal opportunity to participate and that no single individual (including the Facilitators!) dominates the discussion.
- Perceives and responds to differences in the group, such as the level of skills education and comfort with the topic.
- Is aware of cultural and gender issues.
- Encourages participants to answer questions and share expertise.
- Is able to politely bring the discussion back to the point if the group begins to discuss issues beyond the session’s scope.
- Is respectful and non-judgmental of the participants’ ideas and opinions to allow the expression of diverse concerns.
- Sticks to the time – starting on time and ensures adequate time for discussions.
- Obtains feedback and response from the group to provide evaluation mechanisms for the session.
- Provides an appropriate balance of supportive and challenging facilitation to foster learning.
Group Discussion-small group discussions
The advantages of small group discussions include the following:
- Participants have more opportunities to speak and are less likely to be embarrassed compared to a large group.
- The atmosphere is more conducive to share one’s feelings.
- Participants gain self-confidence through sharing information.
- More ideas emerge from the group.
The Facilitator may also ask the group to appoint a Facilitator and a rapporteur. Small group discussions and/or work with pairs should be followed in a large group discussion so that general conclusions can be drawn.
The Facilitator does not lead the group but must be skillful in structuring the discussions so that the stated objectives of the session are accomplished.
It is important to provide clear guidelines for group discussions in advance. These can include:
- Which topics are to be discussed?
- Will the group draw conclusions or make decisions?
- Can opinions or feelings of the participants be shared beyond the small group?
- Will the group be expected to report its discussions to the larger group?
Checklist for the tasks Before /During /After the Training
| Sr. No. | Stage I: Before the training | Yes/No/NA |
|---|---|---|
| A | One month prior to the training | |
| 1 | Training Dates | |
| a | Have I planned training dates in consultation with TISS/CTD/STDC a month prior to the training? | |
| b | Have I checked whether the letter of invitation has been sent to the participants by CTD / SSR to non-NTEP staff at least 20 days before the scheduled training? | |
| c | Have I checked with NTEP participants about the accompanying person and taken the necessary permission for the same? | |
| d | Have I formed the WhatsApp group of the participants and briefed them about the training dates, venue and letter of invitation along with the list of participants for their reference and asked them to get the release order from their DTOs to attend the training? | |
| e | Have I checked whether everyone in WhatsApp group is receiving the messages? Is there anyone whose phone number needs to be updated or included in the group? | |
| f | Have addressed the concerns of the participants regarding the training dates, venue, or issues regarding permissions, request for an accompanying person, special request for leaving early, or not being available for the training? | |
| g | Have I informed the participants to carry their Aadhaar Card and double vaccination certificate while coming for the training? (If applicable) | |
| h | Have I informed the participants that the TA (travel allowance) settlement process will begin only when everyone submits their TA claim forms with necessary documents to the SSR? Additionally, the documentation verification process is time- consuming and TA settlement will take some time. | |
| 2 | Training Venue | |
| a | Have I selected a training venue after considering all criteria like the cleanliness of the training venue, hygienic washrooms, availability of water in washrooms, purified water for drinking, distance from the station etc.? | |
| b | Have I selected a training venue with sufficient space to accommodate the participants? | |
| c | Have I selected a training hall big enough to allow me rearranging of chairs for group work? | |
| d | Have I checked whether the training venue has proper ventilation, power back up and sufficient light? | |
| e | Have I checked whether the training venue has an LCD screen, projector, VGA (Video Graphics Array) cord, whiteboard with stand and duster? | |
| f | Have I checked whether there are enough electrical points for equipment such as a projector and laptops? | |
| g | Have I checked whether the training venue provides good quality food? | |
| h | Have I ensured that the training venue is finalised and booked? | |
| i | Have I checked with the training venue if early check-in is allowed for the participants? | |
| 3 | Invitations | |
| a | Have I completed orientation of STDC and Master Trainers? | |
| b | Have I confirmed with Master Trainers about their level of comfort with the topics and their availability for trainings in next 6 months? | |
| c | Have I sent formal invitations to the CTD to depute participants for the training? | |
| d | Have I sent out invitations to Master Trainers? | |
| e | Does my invitation letter to Master Trainers mention honorarium details? | |
| f | Have I ensured the training material has been shared with the Master Trainers in advance? | |
| g | Do my invitation letters contain the dates, timings and directions related to the training? | |
| 4 | Training Material | |
| a | Please check if you have following with you: A printed copy of the Facilitators’ guide? | |
| b | Copies of Training Agenda/Training Schedule (Soft copies), Translated versions of case studies, group work, skits, statements etc | |
| c | The training kit with pen, notepad, folder, agenda, mask for participants | |
| d | 2 copies of banners | |
| e | Zone wise link for attendance – https://drive.google.com/drive/ folders/103Jf-NalBMMrc0RO6jHeWHI bZ_OBpiDu | |
| f | Zone wise link for Pre and Post Training Assessment questionnaires – https://drive.geogle.com/drive/folders/103Jf- NalBMMrc0RO6jHeWHlbZ_OBpiDu | |
| g | Link to follow social media – https://www.facebook.com/sakshamtiss https://www.instagram.com/saksham_tiss/ https://www.youtube.com/channel/UC3lSzS3nvEAs1MMH0s-Xo2A https://twitter.com/SakshamTiss | |
| h | Link for Feedback form – https://forms.gle/njQYEa73nJK6KEiK7 | |
| i | Check-in- Check-out sheet (if applicable) | |
| B | A week before the training | |
| 1 | Have I created a budget excel file for the planned training batch and got it approved from finance? | |
| 2 | Have I mailed CTD/TISS asking for any specific needs of participants such as ANCs and nursing mothers in terms of accommodation, accommodation need of people coming from long distance, food during fast/travel etc.? | |
| 3 | Have I booked enough rooms for participants at the training venue with a formal email mentioning the date of booking? | |
| 4 | Is the printing and internet facility available at the training venue? | |
| 5 | Do I have details like name, address, telephone numbers, contact person/s of the hotel handy? | |
| 6 | The training needs to display and stick charts on the wall. Have we informed the point person at the training venue about it? | |
| 7 | In case the above-mentioned permission is not given, have I made alternative arrangements? | |
| 8 | Is the brief profile of CTD officials and Master Trainers ready so as to introduce them to the participants? | |
| 9 | Have I finalized the menu and provided a list of participants to the caterer? | |
| 10 | Have I finalised the required audio-visual equipment (computer/ laptop, LCD, DVD player, speakers, microphones, movie clips/films etc.) and kept it ready? | |
| 11 | Have I ensured availability of a person for technical support during the training? | |
| 12 | Have I taken contact number of the person for technical support during the training? | |
| 13 | Am I well equipped with all the stationery mentioned in the stationery list for each session in the manual? | |
| 14 | Have I prepared a first aid box and kept contact details of some clinicians and nursing homes handy in case of any emergency? | |
| 15 | Am I well equipped with appropriate energisers, fillers, activities and relevant movies to energise the participants? | |
| 16 | Have I taken some cash advance for the training? (If applicable) | |
| 17 | Have I received confirmation from Master Trainers about their availability? Do I need to follow-up telephonically in case there is no confirmation? | |
| 18 | Have I had discussions with my team and are the sessions been delegated? | |
| 19 | Have I delegated all these responsibilities? | |
| a | Facilitation of every session | |
| b | Co-facilitation for all the sessions | |
| C | Coordination with STDC | |
| d | Coordination with the point person of training venue caterer/ hotel | |
| e | Stationery | |
| f | Sharing the link for Pre and Post Training Assessment questionnaires on WhatsApp group – https://drive.google.com/ drive/folders/103Jf-NalBMMrc0RO6jHeWHIbZ_OB piDu | |
| g | Sharing the link for attendance – https://drive.google.com/drive/ folders/103Jf-NalBMMrc0RO6j HeWHIbZ_OBpiDu | |
| h | Translations | |
| i | Ensuring attendance of CTD officials at inauguration | |
| j | Registration | |
| k | Welcoming of participants and CTD officials I | |
| m | Fillers/ Energisers | |
| n | Timekeeping | |
| 0 | Taking pictures during the training p | |
| 20 | If training duration includes a holiday, have I ensured the availability of enough support like the opening of training hall on time, technical support for audio-visual equipment, housekeeping staff etc. | |
| 21 | Have I informed the relevant person/s at the training venue that the training may get extended beyond mentioned training timings? | |
| 22 | Have I received participants’ travel reimbursement norms from TISS/CTD? | |
| C | A day or two before the training | |
| 1 | Have I double checked everything and gave reminder calls to/at/for: | |
| a | Training venue | |
| b | Caterer | |
| C | Audio-Visual equipment | |
| d | Technical support for audio-visual equipment | |
| e | Master Trainers | |
| f | Training Stationery | |
| g | Training kit for the participants | |
| h | Banner display | |
| i | Gift hampers (chocolates/chikkis etc.) | |
| j | Participants (regarding training dates, venue and documents required during training) | |
| 2 | Have I organized a welcome note for the participants at the hotel / training venue? (The note has to state the time they need to come in for the registration. Also mention that meals, stay etc. have been provided by the training venue. Any other expenses will have to be borne by the participants. They need to check-out in the morning of the last day.) | |
| 3 | Have I ensured that the caterer is going to provide food as per the contract.? | |
| 4 | Have I ensured a proper welcome of dignitaries (availability of water, tea, snacks, flowers on the dais)? | |
| 5 | Have I designated a laptop for training? | |
| 6 | Are the translations of case studies, statements, stories etc. ready? | |
| 7 | Have I prepared a training folder in which PowerPoint presentations, videos/films, handouts are ready for sessions on all |
| Sr. No. | Stage II: During the training | Yes/No/NA |
|---|---|---|
| A | On the first day of the training | |
| 1 | Training Site | |
| a | Is the training site clean and welcoming? | |
| b | Is all equipment in place? | |
| c | Are the little posters to guide people to the training site and to the toilets displayed at visible locations? | |
| d | Are the training banners put up (at the entrance as well as in the training hall)? | |
| e | Have the meal arrangements been made? | |
| 2 | Training Materials | |
| a | Is check-in and check-out sheet (only for residential participants) ready and kept at reception and being filled by the participants? | |
| b | Is the attendance sheet ready and being filled by the participants? | |
| c | Are the participants receiving training kits on arrival? d | |
| d | Is the film on TISS-Saksham ready? | |
| 3 | Other | |
| a | Am I welcoming the participants? | |
| b | Am I prepared with enough fillers and energisers? | |
| c | Have I shared the Zone wise link for attendance? – https:// drive.google.com/drive/folders/103Jf-NalBMMrc0RO6jHeWHlbZ_OBpiDu | |
| d | Have I shared the Zone wise link for Pre-training assessment questionnaire with the participants? – https://drive.google.com/ drive/folders/103Jf-NalBMMrc0RO6jHeWHIbZ_OBpiDu | |
| e | Have I introduced the training team to the participants? | |
| f | Have I ensured that ground rules for training are formulated? | |
| g | Have I stressed the importance of punctuality? | |
| h | Have I reviewed the training schedule? | |
| B | During the Training | |
| 1 | Is my team present and attentive in the training hall throughout the training to draw links between sessions? | |
| 2 | Has the MET (Monitoring and Evaluation Team) been nominated every day to summarize the previous day’s learning and keep the time? | |
| 3 | Is my team taking photographs of important activities during the course of the training? | |
| 4 | Am I keeping track of the schedule and if it is being followed? | |
| 5 | Am I giving appropriate breaks in between? | |
| 6 | Am I keeping the participants informed about changes in the schedule if any? | |
| 7 | Is there a proper coordination with the caterer? Am I informing them about the changes in menu or the schedule for lunch/dinner/tea if any? | |
| 8 | Have I invited dignitaries (if any) for the valedictory? | |
| 9 | Have I made arrangements for a cultural programme (to be organised in the evening after the second day of training) | |
| 10 | Have I communicated to the point person of the training venue that their team should not be present in the training hall unless requested and can’t be part of this training? | |
| 11 | Am I assuring the participants that necessary annexures/ assignments/handouts will be distributed at the end of the training on WhatsApp? | |
| C | Final day of the training | |
| 1 | Have I ensured that participants residing at the training venue have checked out in the morning? | |
| 2 | Have I taken verbal feedback from the participants about the overall training? | |
| 3 | Have I shared the Zone wise link for post-training assessment questionnaire with all the participants? – https://drive.google.com/drive/folders/103Jf-NalBMMrc0RO6jHeWHlbZ_OBpiDu | |
| 4 | Have I shared the link to follow Social Media? – https://www.facebook.com/sakshamtiss, https:// www.youtube.com/channel/UC3lSzS3nvEAs1MMH0s-Xo2A,https:// www.instagram.com/saksham_tiss/ and https://twitter.com/ SakshamTiss | |
| 5 | Have I shared the link for Feedback form? – https://forms.gle/ njQVEa73nJKGKEiK7 |
| Sr. No. | Stage Ill: After the training | Yes/No/NA |
|---|---|---|
| 1 | Have I submitted all the bills related to food, stay and travel to the finance section at TISS? | |
| 2 | Have I sent check-in and check-out sheet to the finance section at TISS? | |
| 3 | Have I sent the training report to TISS/CTD in the prescribed format and thanked them for their support within two days of the completion of the training? | |
| 4 | Have I kept all courier bills with me for future reference? | |
| 5 | Have I sent an email to the finance officer mentioning the names of all documents I have couriered, copying to all my team members and point person? (date and training details like batch number and training dates)? |

Tata Institute of Social Sciences Saksham Pravaah
Capacity Building for Front Line NTEP Staff on Counselling Soft Skills
Venue: Agenda
| Time | Topic | Name of the Resource Person |
|---|---|---|
| Date: | Day1 | |
| 9.30am -10.00 am | Registration and Pre-Test | |
| 10.00 am – ll.15 am | Introductory Session: Who Are We and Our Aspiration | |
| ll.15 am – ll.30 am | Tea Break | |
| ll.30 am -l.30 pm | Understanding Social Determinants of TB | |
| l.30 pm – 2.30 pm | Lunch | |
| 2.30 pm – 3.45 pm | Enhancing Social Protection Linkages | |
| 3.45 pm – 5.30 pm | Introduction to Counselling and Principles of Counselling (Continue) with Tea Break | |
| Date: | Day2 | |
| 9.30 am – 9.45 am | Recap | |
| 9.45 am – ll.15 am | Stages and Process of Counselling | |
| ll.15 am – ll.30 am | Tea Break | |
| ll.30 am – l.00 pm | Counselling Micro skills | |
| l.00 pm – 2.00 pm | Lunch | |
| 2.00 pm – 3.45 pm | Enhancing Counselling Competencies for TB | |
| 3.45 pm – 4.00 pm | Tea Break | |
| 4.00 pm – 5.30 pm | Enhancing Counselling Competencies for TB (Contd.) | |
| Date: | Day3 | |
| 9.30 am – 9.45 am | Recap | |
| 9.45 am – ll.15 am | Critical Issues in Adherence Counselling | |
| ll.15 am – ll.30 am | Tea Break | |
| ll.30 am – l.00 pm | Our Words, Our Perspectives……. Hamare Shabd, Hamara Nazariya | |
| l.00 pm – 2.00 pm | Lunch | |
| 2.00 pm – 3.30 pm | Going Ahead: Hum Hai Saksham | |
| 3.30 pm – 3.45 pm | Tea Break | |
| 3.45 pm – 5.30 pm | Consolidation and wrap up |
Depending on the state preference the training can also be completed in 2 days.
Please refer to following link for the 2 days agenda for the training –
https://drive.google.com/drive/folders/1NmGgklEd2PESoXOdEcOQl15svlbsPTmb

Saksham Pravaah
Tata Institute of Social Sciences, Mumbai
Pre and Post Training Assessment Tool
https://drive.google.com/drive/folders/103Jf-NalBMMrc0RO6jHeWHlbZ_OBpiDu
Instructions: Please respond to all the questions/items. Please write your response clearly.
Yourresponses will be kept confidential and used for programme purposes only.
[Time: 15 minutes]
[Total Marks = 20]
Background Information:
| Name: | |
| Age: | |
| Sex: Designation: | |
| Educational Qualification: | |
| Work experience under National TB Programme (In years): | |
| District: | |
| State: | |
| Zone: | |
| Date (DD/MM/YYYY): |
Section A
(5 marks)
Instructions: Please read each statement and circle the response which is appropriate according to you.
DO NOT LEAVE ANY STATEMENT UNRESPONDED
| Sr. No. | Responses | TRUE | FALSE |
|---|---|---|---|
| 1 | It is ideal to have a mix of open-ended and closed-ended questions while interacting with TB Patients. | TRUE | FALSE |
| 2 | Giving advice is the most important aspect of TB counselling. | TRUE | FALSE |
| 3 | It is important to give non-verbal cues while the Patient is speaking. | TRUE | FALSE |
| 4 | The gender of the TB Patient will have no bearing on adherence to treatment. | TRUE | FALSE |
| 5 | Confidentiality and an informed decision-making process are paramount when counselling TB Patients and their family members. | TRUE | FALSE |
Section B
(10 marks)
Instructions: Please read each of the statements given below. Using a four-point rating scale, state the extent to which you agree or disagree. Circle the response which is appropriate for you. Please remember that there are no right or wrong answers to these statements. You can express your opinions freely.
DO NOT LEAVE ANY STATEMENT UN RESPONDED
| l. | Patients can be scolded if they do not listen. | (1) Completely Agree (2) Somewhat Agree (3) Somewhat Disagree (4) Completely Disagre |
| 2 | Visiting TB Patient’s homes can be threatful | (1) Completely Agree (2) Somewhat Agree (3) Somewhat Disagree (4) Completely Disagree |
| 3 | Adherence to treatment is more important than the mental health of TB Patient. | (1) Completely Agree (2) Somewhat Agree (3) Somewhat Disagree (4) Completely Disagree |
| 4 | TB Patients need sympathy rather than empathy. | (1) Completely Agree (2) Somewhat Agree (3) Somewhat Disagree (4) Completely Disagree |
| 5 | Patients are lazy therefore they don’t come to the Primary Health Centre to collect their medicines. | (1) Completely Agree (2) Somewhat Agree (3) Somewhat Disagree (4) Completely Disagree |
| 6 | NTEP (National TB Elimination programme) staff do not have time to speak to all of their Patients because they have a very heavy Patient load | (1) Completely Agree (2) Somewhat Agree (3) Somewhat Disagree (4) Completely Disagree |
| 7 | It is a woman’s duty to take care of her husband who is a TB Patient | (1) Completely Agree (2) Somewhat Agree (3) Somewhat Disagree (4) Completely Disagree |
| 8 | TB Patients should not eat together with their family members. | (1) Completely Agree (2) Somewhat Agree (3) Somewhat Disagree (4) Completely Disagree |
| 9 | NTEP staff do not get into the details of the regimes with illiterate Patients as they will not understand it. | (1) Completely Agree (2) Somewhat Agree (3) Somewhat Disagree (4) Completely Disagree |
| 10 | Getting married is difficult for TB Patients. | (1) Completely Agree (2) Somewhat Agree (3) Somewhat Disagree (4) Completely Disagree |
Section C
(Total 5 Marks)
Instructions: Please read each of the statements given below. Circle the response which is appropriate for you.
DO NOT LEAVE ANY STATEMENT UNMARKED.
| 1 | Which of these is not a micro skill for conducting a counselling session? | (1) Active listening (2) Questioning (3) Using silence (4) Sympathy |
| 2 | Select the most important documents required for Pradhan Mantri MatruVandana Yojana for the initial enrolment from the options: | (1) PAN Card and Bank Passbook (2) Aadhaar Card and Marriage Certificate (3) ANC Card and Marriage Certificate (4) ANC Card and Bank Passbook |
| 3 | An effective Counsellor should not be – | (1) Self-confident (2) Empathetic (3) Judgmental (4) Trustworthy |
| 4 | While listening to a Patient, a Counsellor should – | (1) Narrate their own experience (2) Show empathy to the Patient (3) Advise on ethical behaviour (4) Establish a personal relationship with the Patient |
| 5 | From the statement below identify the type of question it is:Counsellor: “You are taking your medicines regularly. Aren’t you? Patient: “Yes”. | (1) Open-ended question (2) Closed-ended question (3) Leading question (4) Mixed question |
Thank you!!
Introductory Session Who Are We & Our Aspirations!
Introductory Session
Who Are We
& Our Aspirations!
SESSION

Session Overview

Activity 1 : Coming to the Training
Activity 2: Jab We MET – Forming a Monitoring and Evaluation Team
Activity 3 : Setting Ground Rules
Activity 4: Expectations from the Training
Activity 5 : Triad interview to enable self-assessment of Counsellor/ NTEP staff
Activity 6: Introduction to TB
Activity 7: Pre-Training Assessment Test
Session Objectives

Learn each other’s names and get familiar with each other
Agree on a set of rules during the training for the participants to follow Understand the programme and to clarify any misunderstanding of the training programme.
Time allowed
2 hours
Material required

IJ Film on Saksham
IJ PowerPoint presentation
IJ Whiteboard markers, chart papers, pens and notepads
1J Stickers for ground rules
IJ Chart paper with the figure of a tree (Refer to Annexure)1J Sticky notes for participants
Method
Go through the background of Saksham Project in the Facilitator’s guide. Check the Film on Saksham.
Familiarise yourself with the available information about the profile of the participants well in advance.
Get yourself oriented to the training framework.
Familiarise yourself with the National Strategic Plan (NSP)2020-2025.

Coming to the Training

You as a Facilitator will –
Welcome all the participants. Tell them that – “This is the first time that Saksham Pravaah, is intended to train front line NTEP staff who are new to the concept of Counselling . We hope that this training would be a learning experience for each one of the participants.”
Orient them about TISS and Saksham Project by using the Film on Saksham. Tell the participants that- “We all have been sent by our states or by our STOs DTOs for these trainings. But the training will be effective only when we come for it voluntarily. For this, let’s go out and re-enter the training hall to attend the training by our own will!”
Before going ahead, take all participants out together. Ask them to stand in a circle and close their eyes and repeat aloud – “Here, I am keeping all the burden, tension, stress, anger, anxiety, fear and all kinds of negativity outside the training hall and entering it with lots of positive energy, enthusiasm and motivation to revise and learn from each one.”
Next, bring all participants into the training hall and ask them to stand behind their seats. Now, ask each one of them to call out their name, from where they are and say, ‘I am coming to the training!’
While each one introduces themself, Facilitator will welcome that person by taking their name and requesting them to be seated.
At the end, the Facilitator will also introduce themself and will sit in the same manner as others and will welcome all, once again.

Jab We Met – Forming a Monitoring and Evaluation Team

Following the participatory principle of the training, participants will monitor the progress of the daily sessions by recording significant processes and learnings to give a recap the following day. For this, the Facilitator will ask for two volunteers – the first volunteer will record the day’s proceedings, and using an innovative method, provide a recap the next morning; the second volunteer will keep the time, and ensure that everyone, including the trainers, will follow the timeline. (Continue this practice every day- form the MET every morning immediately after the recap is over).

Setting Ground
Rules

This activity will help in making a smooth path to a successful training
The Facilitator will ask the participants to identify behaviours that could hamper and/or interrupt the training.
The Facilitator will request the timekeeper from MET to write these behaviours in BOLD letters on a fresh chart paper without any repetition.
The Facilitator will ask for assent from participants to ensure that they will avoid/ prevent such behaviour. This will be done by asking for solutions to each of the barriers. For example- ‘can we use the mobile phones during the breaks so as to not disturb the training?’ or ‘will you raise your hand to ask for permission to speak instead of many participants speaking simultaneously?’ etc.
As a ground rule, Facilitators will request the participants to desist from taking selfies during the training, inside the training hall.
In case it does not emerge from the participants themselves, the Facilitator should mention a ground rule about not disclosing the Patient’s identity and keeping all discussions confidential.
The chart will be displayed for all to see and follow throughout the training period. Alternatively – Facilitators will motivate all participants to formulate the ground rules using the above method but instead of writing them on a chart paper, use stickers with messages , Such as, ‘be punctual’ , ‘ keep your mobile phones on silent mode’ etc. and stick them on a chart paper, one by one after the discussion.

Expectations from the Training

To help participants understand the programme and to clarify any misunderstanding about the training programme, you as a Facilitator will conduct the following activity –To help participants understand the programme and to clarify any misunderstanding about the training programme, you as a Facilitator will conduct the following activity –
Mount a chart paper on the wall with the figure of a tree on it and tell the participants that this is an ‘Expectation Tree’. Each one of you might have come here with some expectations from this training. Now everyone will write on a sticky note what your expectations are from the training? What do you want to learn in these three days of training?
Distribute the sticky notes for them to write on and ask them to stick them on the figure of the tree by taking turns.
Tell the participants that this is the first session of the three-day training. The session intends to help the participants to get to know each other and be informed of the overall aims of the training and the schedule for the three days.
Quickly go through the training agenda. Tell the participants that they are free to share their individualised experiences through the course of the training since this would help them gain clarity as well as prove to be a learning opportunity for others.

Triad Interview to Enable Self-Assessment of Counsellor/NTEP Staff

You as a Facilitator will –
Tell the participants that we will have an exercise to know each other better. Ask participants to pick up their notepads and pens and stand in an ascending order based on their height. The first three in the line would form the first triad and subsequently the next three the next triad till onereaches the end of the line.
Now introduce the concept of triad interview. Demonstrate it with the first triad for everyone to understand the process clearly. Illustrate how participant A will interview participant B while participant C will document the interaction. Similarly,
while B interviews C, documentation would be done by A, and while C interviews A, documentation would be done by B. The roles would be switched every 4-5 minutes so that each group member performs all three roles. This way every group member would take turns to become interviewer, interviewee, and rapporteur.
Write the following questions on board and tell the participants that the questions displayed on the board should be covered in the interview. The interviewer should spend not more than one minute per question.
Slide No. l
- Profile: Name, Qualifications, Years of Professional experience
- What in your view is your biggest strength being in this profession?
- Do you find it difficult to work with anykind of Patients/issues?
- Which song describes you the best?
Once the interviews are completed, one after the other, ask all members to introduce an interviewee when they were rapporteur or were responsible for documentation. Then the person who is introduced will be asked to sing the song that describes them best. Then they will introduce the next person in the same manner. After a couple of presentations, there is likely to be a repetition of points. In case of repetition, ask the presenters to share only additional points that they may have.
Facilitators should keep jotting down the common points in the notepad for future reference during the training. Ensure that you do not spend more than 10 minutes on the sharing.
Bring to the fore – ‘the wealth of experience’ present in the group! Tell the participants that it is an amazing experience to be in this training hall, if we add the years of experience of everyone present, then this hall contains of more than hundred years of experience. Hence, we will not be teaching anything, instead learn from each other by sharing our experiences.

Introduction to TB:
(PowerPoint Presentation)(This activity can be skipped if the participants belong to NTEP)

Facilitators will introduce the activity by saying – Now let’s understand what TB is, what are the types of TB and the treatment available for TB. The Facilitator will conclude the session with a Power Point Presentation on Introduction to Tuberculosis (TB). (Refer to PPT on Introduction to TB). To avoid the use of PPT Facilitator can use chart papers / use whiteboard to write and discuss the main points. Link for the PPT and PDF on Introduction to TB :
https://drive.google.com/drive/folders/17Oid7xhxFAGh0p2wyieU4JVsf4DYmUVh

Pre-Training Assessment

At the end of this session, Facilitators will share the link for Pre-Training Assessment and ask the participants to fill it up. Instruct them that they need not worry about this Pre-Training Assessment and answer it without fear. There might be some questions which they may find difficult to answer, but, be assured that these will be covered in the three days training and same questions will be asked in the Post-Training Assessment Test, on the last day of the training. Hence, it is not an evaluation of the participants, but the evaluation of the training. Facilitators will assist if any technical support is required or if any of the words are not clear to the participant.
Link for Pre -Training Assessment tool – https://drive.geogle.com/drive/folders/103Jf-Nal BMMrc0RO6jHeWH IbZ_OBpiDu
Annexure
Annexure
Example of an Expectation Tree
Understanding Social Determinants of TB
Understanding
Social Determinants
of TB
SESSION

Session Overview

Activity 1 : Introduction to the Session
Activity 2 : Truth of the Matter – Social Construction of Gender
Activity 3: Storytelling: Hum Saath Saath Hain…
Activity 4: A piece of my Sky – Power Walk
Master Trainers required for this session: CBS/ Ex-Saksham Master
Trainers/ Prerak staff/ Faculty/ past experience in HIV/ TB training.
Session Objectives

By the end of this session, participants will be able to:
Understand structural factors and social determinants that make individuals vulnerable to TB and influence diagnosis and treatment adherence.
Understand the Social Construction of Gender and enumerate the Difference Between Sex and Gender.
Appreciate the linkages between addressing the social determinants and achieving the goals of the National TB Elimination programme (NTEP).
Time allowed
l hour 30 minutes
Material required

CJ Whiteboard and markers
Method
Preparation before the session:
You as a Facilitator will –
Ascertain a space for the ‘Power Walk’ activity. This activity will need a large area that can accommodate approximately 20 or more participants. (The space could be either indoors or outdoors).
Get the details of the participants, viz. age, qualification, and years of experience from the training co-ordinators. These details will be required to frame the questions for the ‘Power Walk’ activity. Alternatively, you as the Facilitator can begin this session with a brief round of introduction where the participants will be asked to introduce themselves on the aforementioned details.

Making the Connections

You as a Facilitator will –
Start the session with brainstorming on social aspects that are driving the TB epidemic and also affect TB diagnosis and treatment adherence.
Jot down the points shared by the participants on the whiteboard. Write Poverty, Education, Stigma, and Discrimination, as they come up at the top of the board, and the remaining points such as addiction, unemployment, etc. at the bottom of the board.
Probe further and encourage participants to come up with stigma and discrimination and Gender as a social driver.
Ask participants if they have heard of the term “Gender” and if yes, what it means. Note the responses on the white/black board. More often than not, gender will be explained interchangeably as “sex”.
Ask the participants what is the difference between “sex” and “gender”.
Don’t get into a discussion at this point of time and inform the participants that you will now undertake an exercise which will provide clarity on this issue.

Truth of the matter – Social Construction of Gender

Label two opposite walls as ‘Biology Wall’ and ‘Social Wall’
Ask the participants to stand in a straight line at the centre of the room, equidistant from the labelled walls.
Inform the participants that after each statement, participants have to move towards the Social Wall or the Biology Wall depending on whether they feel that the statement is based on socio-cultural factors or has a biological basis. For e.g., the statement, “The colour of the hair of the majority Indians is black” has a biological basis i.e. it is innate, or one is born with it, as against “There is Son preference in India” is based on social-cultural factors and does not have any biological basis. Inform the participants to reflect on each statement and decide individually as they are asked to justify the reason why they have chosen a particular wall. Also, ask them to choose either but not to be on the fence or choose the midpoint.
Refer to the list of the statements outlined in Annexure l and read aloud one statement at a time. Have participants discuss their views about all the statements and explain to one another why they felt a certain way about each statement. Ask the participants to come back in to the line after each statement. You as the Facilitator have to play a neutral role during the exercise and encourage the participants to explain their points and convince their fellow participants of their views.
Ask all the participants to take their seats after all the statements are read and once again ask them what is the difference between “Sex” and “Gender”.
Keep in mind the purpose of the activity, which is to help participants differentiate between what one is born with and what is socially constructed.
Read all statements beforehand and prepare responses to anticipated arguments. Asking participants why they felt the statements have a biological basis and what negative effects these stereotypes can have, may help them understand the importance of being aware of gender as a social construct.
Assure the participants who are confused or are not sure, that it is ok to be in that position and this is an opportunity to probably unlearn and gather a newer perspective.
Key points to emphasise:
| SEX (Biological) | GENDER (Social) |
|---|---|
| Sex refers to the biological difference between males and females. Sex can also be used to describe physical acts of sexual intercourse. | Gender is a social construct and refers to the economic, social and cultural attributes and opportunities associated with being male/masculine or female/ feminine. |
| Sex is innate (inborn) and will remain the same in a particular social setting and time. | Gender roles and behaviour are assigned by society and are learned rather than being innate (inborn). |
| Since gender is not innate/biological, it can change over social settings and time, for example, the status of women in India is different from the women in USA or the Middle Eastern Countries. Similarly, the freedom that women in India enjoy today is different from what was enjoyed by our grandmothers. |
- Boys and girls are systematically taught to be different from each other. Socialisation towards gender roles begins early in life and are learnt from the family, school, friends and media.
- This includes learning to be different in terms of appearance and dressing (girls have long hair), behaviour, activities and pastimes (girls are given dolls/kitchen set as gifts), emotions (boys are taught to be tough and to not cry like a girl) responsibilities (men are the providers) and intellectual pursuits.
- These fixed gender roles can affect both men and women negatively.
- Men are expected to be the providers and hence are expected to be mentally and physically strong as they have to take care of the family.
- Men are therefore supposed to eat healthy and also seek medical attention immediately if they are ill. Both nutrition and health seeking behaviour have a gender basis.
- There is a biological difference in the sexual organ and the reproductive functions between men and women. However, this biological difference is underlined and used to differentiate between and control both men and women.
- As TB Counsellors, it is important to differentiate between what is biological (by birth) and what society has decided for men and women. For example, ‘women are better cooks’ has no biological basis. Similarly, ‘Boys do not cry’ is a social construct without a biological basis.
- Counsellors also need to refrain from perpetuating gender stereotypes like- women are weak, men are strong etc. Also, no public messages should be given in counselling such as- ‘Look at your children. Who will look after them if you die. You have to live for them’, etc.
- Most importantly, Counsellors need to understand that since gender norms are learned (not inherited at birth), it can be unlearned
Source:
Adapted from Activity 1, Session Three on Social drivers of HIV epidemic – Gender, Sex and Sexuality – A Manual for Facilitators by Skill-Based Training for ICTC, STI and ART Counsellors -A Facilitators’s Guide (Counsellor Contact Training or CCT) by Saksham Prerak.

Understanding Gender Norms, Roles and Relationships

Facilitator will introduce the topic by saying –
Gender norms and roles contribute to the establishment of gender relations. Gender relations are the social relations between and among women and men. In other words, they set out how women and men should interact with each other – and among themselves.
Gender relations determine hierarchies between groups of men or women based on gender norms and roles.
For example, in many households, older men often hold decision-making authority. This in turn contributes to unequal power relations, access to and control over resources.
As an example, explain the structure of a joint family in the Indian context. Ask the participants to imagine a household where a couple has 4 children, an elder son followed by a daughter and two sons. All of them are married.
Facilitator can either use picture from the Bollywood Movie Hum Saath Saath Hain or alternatively, draw a Pedigree chart as below:
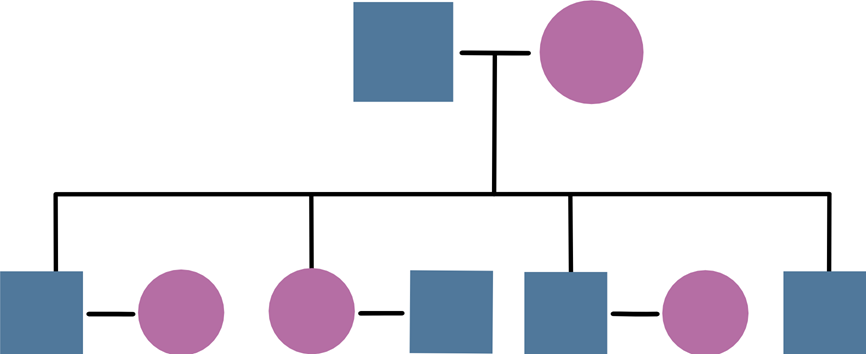
Then ask questions and elicit from the participants to rank who has most decision making power, access to and control over the resources. In this family, the father has more power over the sons, but the sons might enjoy more power and have higher decision-making power over the mother and other women in the family. The mother might be lower in the hierarchy but can exercise more power and take decisions over her daughters-in-law. The sister-in-law might have lower power/decision-making in her marital home but has more say in the decision-making in her maiden family.
Now connect it to TB and see how the youngest daughter-in-law might have access to TB information, diagnosis, ADR care. Also, does she have decision-making power for reproductive issues or access to nutrition? What about the Bank account for DBT?
As TB Counsellors/NTEP staff, it is important to understand Gender as a social construct and how gender norms increase vulnerability to TB.
TB prevention, care and treatment counselling will not be effective unless we address gender issues.
TB Counsellors/NTEP staff need to use a “gendered lens” to understand TB prevention and treatment. Very often, options like condom-use are discussed with the women as a contraceptive method without understanding the amount of decision-making power they have in the household. Counsellors/NTEP staff need to provide “gender sensitive counselling” and involve the spouse in the counselling. There might also be a need to involve the mother-in-law or sister-in-law in nutrition counselling.
Key points to emphasise:
- Structural and social factors, such as poverty, gender inequality and human rights violations increase people’s vulnerability to TB infection and impact diagnosis and treatment.
- These factors are beyond the control of an individual and operate at different societal levels to influence individual risk and to shape social vulnerability to infection.
- In the case of TB, poor ventilation and overcrowding in homes, workplaces and communities increase the likelihood of uninfected individuals being exposed to TB infection.
- Individuals with TB symptoms, such as persistent cough, often face significant social and economic barriers that delay their contact with health systems where an appropriate diagnosis might be made. These include difficulties in transport to health facilities, fear of stigmatisation if they seek a TB diagnosis and lack of social support to seek care when they fall sick.
- There is a need to move away from a bio-medical and disease control approach to a more psychosocial approach.
- The issue of treatment default cannot be viewed in isolation from the social determinants and there is an urgent need to strengthen the focus on psychosocial intervention within the TB Treatment and Care programme.

A Piece of My Sky

Refer to picture relating to power walk in Annexure 2
After the discussions on the social drivers of TB, inform the participants that you will now conduct an activity called ‘Power Walk’.
Inform the participants that this activity will be conducted to further understand the social drivers of TB.
Move the participants to the space designated for this activity.
Ask the participants to stand in a horizontal line and hold hands. The participants should be facing the wall/solid structure and there should be some distance between them and the wall.
Inform the part1c1pants that you will be reading a list of questions listed in Annexure 2. If they feel that the answer is ‘yes’, they need to take one step forward and if the answer is ‘no’ they need to move one step backwards. The questions are about the participants themselves and hence they will have to move either forward or backward. The Facilitator will stress the fact that the participants do not have an option of not moving; the participants will have to either move forward or backward on every question.
Inform the participants that they have to hold hands for as long as possible.
After reading all the questions, ask the participants to look around at the others in the line and observe the following:
Who is still holding hands?
Who is ahead of the others in the line?
Now ask the participants to run and grab a space for themselves against the wall. Following this, ask the participants to assemble back into the training hall.
Ask the participants to share their experiences of doing this activity: How did they feel when they had to take a step backwards?
How did it feel to let go of hands?
At the end of the activity, who was nearest to the wall and who was the farthest?
What does this say about the opportunities that are available to some and not to others?
Who could grab the wall? Who could not?
Did anyone try to accommodate others so that they could also touch the wall? Do we take our privileges for granted?
Were there any participants, who did not try to run towards the wall at all? If yes, why?
How did they feel to be moving backwards and about being last in the line without doing anything to be in this position?
Could they draw any connections between this exercise and the previous discussion on social drivers?
Key points to emphasise:
- If the finish line is equated to accessing TB care or completing TB treatment, highlight how social determinants (sex, religion, education, financial and job security) influence these factors.
- As seen in the activity, people with greater opportunity owing to either their sex, religion, class, caste, gender, educational status, occupation get ahead of the people who are ‘left behind’ or marginalised.
- It is important to understand that structural factors are beyond the control of individuals and will intersect (sex, gender, caste, class, sexual identity, educational status and financial aspects) to increase vulnerability of a particular group and community to illness like TB, HIV and access to treatment and health services.
- Being infected with TB and intersection with gender, class, caste will further increase the stigma and discrimination, thus creating multiple layers of stigma and discrimination which will affect treatment seeking and treatment completion.
- Therefore, it is important for NTEP workers to take additional efforts to reach out to the individuals who are way behind (due to social determinants) and bring them closer to the finish line (i.e., treatment completion).
- It is important to address the social drivers if we want to achieve the goals of the NTEP programme.
- Linking Patients to social security schemes offered by government as well as non governmental organisations can be one way of mitigating structural factors which may lead to delay in diagnosis and/or treatment default.
- Inform the participants that the ways to enhance linkages to social protection schemes will be covered in detail in the last session.
Questions on Understanding Social Determinants of TB

- TB Patients who are chronic alcohol consumers have higher tendency
To initiate treatment early
To complete treatment
To become lost to follow-up - Although TB is an air-borne infection , social determinants increase a person’s vulnerability to TB infection, impact, diagnosis and treatment.
Correct
Incorrect
Annexure 1
Truth of the matter – Social Construction of Gender
List of statements:
- Girls are delicate, boys are not.
- Boys’ voices break at puberty.
- A wife should earn less than her husband.
- Boys do not cry.
- Women can get pregnant, men cannot.
- Women are better cooks than men.
If the Participants seem to have higher awareness about gender, you can use the following additional statements:
- Men make better drivers than women.
- Women have maternal instincts.
- Men are good at logical and analytical thinking.
Link for Annexure lfor Hindi translation of statements for activity Truth of the matter
https://d rive.geogle.com/d rive/folders/19U2p-lZEl6wqp c7 xwedBiZkkoj60nxM
Annexure 2
List of questions for the Facilitator for Piece of the Sky Activity: (Not to be photocopied)
- 1. Are you a male?
- 2. Do you have an Aadhaar Card?
- 3. Are you married?
- 4. Do you have a male child?
- 5. Do you have a post graduate degree?
- 6.Do you have a permanent job?
- 7.Do you live in your own house?
- 8.Do you own a four-wheeler?
- 9.Do you hold a passport?
- 10.Do you have medical insurance?


Link for Annexure 2 for Hindi translation of statements for activity Piece of the Sky https://drive.geogle.com/drive/folders/19U2p-lZEl6wqp c7xwedBiZkkoj60nxM
Understanding Social Protection Linkages
Understanding
Social Protection
Linkages
SESSION

Session Overview

Session objectives
Activity 1 :
Vulnerability mapping and use of checklist, Haqdarshak App orother Apps as a directory of social protection schemes
Activity 2:
Needs assessment of Patients and their family members using case studies
Summarisation
Master Trainer required for this session: Master Trainer who has previous experience of undertaking Gol Linkages or aware of the schemes at the state viz. Vihaan staff/HIV Counsellor/COO/Field Officers from Ministry of Social Justice and Empowerment/Saksham DR-TB Counsellors in Maharashtra/ Gujarat/ Rajasthan / Karnataka.
Session Objectives

Understand the need of linking Patients to various social protection schemes. List the socially and clinically vulnerable groups among Patients.
Understand various challenges experienced by each group in accessing social protection services.
List existing central and state government schemes specific to each group.
List the potential donors (individuals, NGOs, Trusts and companies who can support under CSR) for nutritional support to Patients.
With the help of a checklist, understand the prerequisites and benefits of each scheme.
Discuss the benefits of using the checklist for Patients as well as for the effective implementation of the national programme. Get acquainted with Haqdarshak, an online App for checking eligibility to various social protection schemes.
Time allowed
l hour 20 minutes
Material required

IJ Whiteboard markers
IJ Chart papers
IJ Projector and laptop
Method
Session Objectives (5 minutes}: Discuss the objectives briefly

Vulnerability Mapping and the use of Checklist, Haqdarshak App or other Apps as a Directory of Social Protection Schemes

You as a Facilitator will –
Introduce the topic by asking Participants who are the vulnerable groups among TB patients. For this, they can recall the discussion during the previous session on Determinant of TB.
Then divide the participants into four groups.
Draw the following format on the whiteboard which is to be used for this group work.
| Sr. No. | Vulnerable groups | Reasons | Government schemes |
|---|---|---|---|
Now ask participants to think of various vulnerable groups among TB Patients, reasons for their vulnerability, existing government schemes for each of them and write them on their chart papers.
Explain the table giving an example of a PLHIV. Explain why do we call them a vulnerable group. What are the social and medical risks associated with HIV along with existing schemes for them?
- Ask the participants to refer to the Annexure 2 handout for the checklist of linkages. Take the participants through some of the schemes, documents required, eligibility criteria, benefits, whom to contact for each scheme and discuss how to use the checklist during the course of the treatment.
- Introduce the participants to Haqdarshak App- Open the Haqdarshak App in the phone and request them to log in and take them through all the functions by clicking all applicable tabs.
- Discuss the significance of this app- Not all of us are aware of all the existing schemes across various fields, such as health, livelihood, housing etc. so this app, after feeding in basic demographic information gives a comprehensive list of schemes to which a person is eligible. Further, it also shows the required documents and concerned authorities.
- Whenever staff meets the Patient, either at health centre or during a home visit, they should use this app, access the eligibility and assist the Patient in linkages.
- Please instruct the participants to install the app in their phones and to go through it so any query can be addressed
during the training itself. - Lastly, demonstrate to them the State Government site and how to navigate to locate the hubs to gain documentary proofs in their area. These documentary proofs are required while availing various government schemes. (In case of Maharashtra – https://aaplesarkar.mahaonline.gov.in)
- Now, tell the participants that they will get 10 minutes to prepare and 5 minutes to present. One member from each group should present. Written chart papers should be displayed on the wall.
- While presenting, request the participants not to repeat the schemes discussed by previous groups, but to discuss in detail schemes other than that.

Needs Assessment of TB Patients and their Family Members using Case Studies

- Share with the participants cases from Annexure l on the What App group.
- Assign one case to each group.
- Ask them to discuss in the group and identify what all schemes will be applicable to the Patient and his/her family members.
- Ask one participant from the group to read out the case for all.
- Then ask the remaining participants from the same group to identify and share with everyone the schemes which will be applicable to the Patient and his/her family members.
Ask other groups, if they want to add anything more which was not covered by the group. sum up the schemes for the case and go to the next group for the next case.
Questions on Understanding Social Determinants of TB

- A male TB Patient, aged 22 years, works as a street vendor and has an Aadhaar card . From the options given below, select one most suitable social protection scheme applicable for him.
I. PAN card
II. E-Shram Card
III. Caste Certificate
IV. PM Kisan Sanman Yojana - A female PLHIV-TB aged 35 years who is a widow, lives with her 5-year- old child. From the list of schemes mentioned below select TWO most beneficial social protection scheme options applicable for this family:
I. Bus concession pass
II. Widow Pension scheme
III. Mid-day meal programme
IV. Bank account
Annexurel Case Studies
Annexurel
Case Studies
Link for Hindi translation of Case studies and Handout on Checklist for Social Protection Schemes https://drive.google.com/drjve/folders/lupOZPh9tFKUBE9dNMuRiUlswjfHfXXts
Case study 1:
A female Patient named ‘A’ lives in village ‘B’ which is 20 km away from the nearest PHC and 40 km from DTC. ‘A’ has MDR and is also co-infected with HIV. She is widowed and lives with her son, daughter-in-law and a newborn baby. When told about the provision of DBT, it was observed that she doesn’t have a bank account.
Case study 2:
Patient named ‘X’ recently met with an accident and has lost one of the lower limbs. He has lost his job as well due to disability and now does not want to continue the treatment. He lives with his 25-year-old son who is a government servant.
Case study 3:
A female Patient is four months pregnant and lives with her husband and a 3-year old daughter in a small village in district ‘A’. The husband is not able to apply for a government job as his caste certificate is misplaced. He is the sole earning member of the family.
Case study 4:
A Patient named ‘D’ has a post-graduate degree and is looking for a job. He has been staying in this state since birth but doesn’t have a domicile certificate because of which he is not able to apply for jobs. He stays with his parents and a sister who is a divorcee.
Annexure2
Annexure2
Handout: Checklist for Social Protection Schemes
| Criteria | Name of the scheme | Website | Where will you get the information? |
|---|---|---|---|
| Is the Patient from a rural area? | Mahatma Gandhi Rural Employment Guarantee Scheme | http://nrega.nic.in/netnrega/home.aspx | Grampanchayat office |
| Does the Patient have caste and marriage certificate? | Caste and marriage certificate | Marriage registration office at district HQ/ Tehsil office | |
| Is Patient or caregiver between theage of 18 to 40 years and not a taxpayer | Pradhan Mantri Atal Pension Scheme Shramayogi Mandhan pension Yojana (only for unorganised sector) | http://pmjandhanyojana.co.in/atal- pension-yojana/ | Any nationalised bank |
| Is Patient or caregiver between the age of 18 to 50years | Pradhan Mantri Jeevan Jyoti Beema Yojana | http://pmjandhanyojana.co.in/jeevan- jyoti-bima-yojana- pmjjby/ | Any nationalised bank |
| Is Patient or caregiver between the age of 18 to 70years | Pradhan Mantri Suraksha Beema Yojana | http://pmjandhanyojana.co.in/suraksha- bima-yojana/ | Any nationalised bank |
| Is Patient or any member of the family a widow? (age 18 to 60 years and for BPL families} | Widow Pension scheme | https://pradhanmantriyogana.in/category/widowpension- scheme/ | Forms available online |
| Is the Patient or caregiver pregnant or breastfeeding? | Pradhan Matri Matru Vandana Scheme | https://pradhanmantriyogana.in/prad ha n-ma ntrimatritva-vandana-yojana/ | PHC, Anganwadi, civil hospital. Forms available online |
| Is there a newborn in the family? | Birth certificate | Vital registry at district HQ or Tehsil | |
| Is there a child between ages of 6 months to 6 years | Take Home Ration (THR} | Anganwadi (For THR} | |
| Any TB Patient | Bus concession in state transport | Bus depot | |
| Is Patient or caregiver disabled? | Disability certificate and disability benefits | District collector office / State Social Justice Department |
Introduction to Counselling and Principles of Counselling
Introduction to
Counselling and
Principles of Counselling
SESSION

Session Highlights:

Session overview
Activity 1 :
Activity 2:
Activity 3:
Being an effective Counsellor
Rapid Fire Round
Understanding Principles of Counselling
Session recap and Key messages
Session Overview

Counselling in the area of Tuberculosis ranges from awareness to treatment adherence for successful treatment completion. Counselling also helps to combat stigmatisation and discrimination against TB. It helps in prevention of TB by creating awareness and correcting common misconceptions about TB among Patients and their families. It facilitates linking Patients to testing services. This session is an introduction to the meaning and definition of counselling and essential counselling principles and ethics to be followed by a Counsellor/ NTEP staff in counselling. This session will give opportunity to the Counsellor/ NTEP staff to explore one’s principles and thus to lead effective Counselling service delivery.
Master Trainer required for this session: Faculty of Social Work/Ex-Saksham Master Trainers/Prerak Staff/Faculty of Psychology/ CBC. Master Trainer who has some counselling practice experience will be required. Ideally, this session, session on Stages and Process of Counselling and session on Counselling Micro Skills should be conducted by the same MT or a pair of MTs.
Session Objectives

By the end of this session, participants will be able to:
- Understand what Counselling is.
- Understand what Counselling is not.
- Understand the qualities of an effective/good Counsellor/NTEP staff.
- List the principles of Counselling.
Time allowed
2 hours 15 minutes
Material required

CJ Chart Papers
CJ Pen/Pencil/sketch pens
CJ Whiteboard marker
CJ Chart Paper cut out in a human shape
CJ Copies of Annexure- Handout/ Or soft copies of same can be shared with the participants
Method

Matters of the Heart
(Hamare Dil Ki Baat)

You as a Facilitator will –
Ask the participants to recall a difficult time in their life when they felt sad, ashamed or guilty.
Ask the participants if they have ever talked to someone (e.g. a friend, relative, mentor or Counsellor) about it?
Sometimes talking to someone makes us feel better, but it can also make us feel worse!
Divide the participants into 4 groups.
Ask Groups 1 and 3-
What qualities in that person helped you feel better, take wiser decisions and make healthier choices?
Please list the qualities of such a person or what the person did to help you. You do not have to describe the ‘event’ that made you feel good.
Ask Groups 2 and 4-
What qualities in that person made you feel worse, lose hope, feel ashamed / guilty/demoralised/angry, or make unhealthier choices?
Please list the qualities of such a person or what the person did that made you feel worse.
You do not have to describe the ‘event’ that made you feel bad. Ask Groups 2 and 4 to present first followed by Groups land 3.
The Facilitator will note the points in 2 columns on the board or in a word document and conclude that column l is what is not counselling and column 2 is what Counselling is.
After this activity have a quick brainstorming on what is counselling and consolidate the discussion by using the following key points.
Alternatively, Facilitator with the help of one of the participants can demonstrate a role play portraying negative qualities of a Counsellor. All Participants will have to note these negative qualities and share them with the Facilitator after the role play. Facilitator will conclude by summarising what is not counselling and thus will outline what is counselling.
Key Learnings:
Counselling is an interactive process characterised by a unique relationship between the Counsellor and the client that leads to a change in the client in one or more of the following areas:
I. Behaviour
2. Level of Emotional Distress
3. Beliefs
• Counselling is a professional relationship that empowers diverse individuals, families and groups to accomplish mental health, wellness, educational and career goals. (David M. Kaplan, Vilia M. Tarvydasand Samuel T. Gladding, 2014)
• Counselling involves supporting individuals to take charge of their own lives by providing information, facilitating emotional adjustments and enhancing mental health. Enabling them to understand and accept the problem, develop resources to take adaptable and realistic decisions and alter their own behavior to produce relatively enduring and desirable consequences.
• Counselling is:
Specific to the needs, issues and circumstances of each individual Patient An interactive, mutually respectful and collaborative process
Goal-directed
Oriented towards developing autonomy, self-responsibility and confidence in Patients
Sensitive to the socio-cultural context
Eliciting information, reviewing options and developing action plans Inculcating coping skills
Facilitating interpersonal interaction
Bringing about attitudinal change
• Counselling is not :
Telling or directing Giving advice
A casual conversation An interrogation
A confession
Praying
• Some common errors in counselling
Judging and evaluating
Moralising and preaching
Labelling
Unwarranted assurance
After concluding the previous activity, mention that now it is established what Counselling is and what Counselling is not. Counselling is not just talking. It follows certain principles, goes through certain stages and processes and has a set of certain skills as micro-skills. From hereon we will try to understand more about counselling. In the next session, we will also understand and practice Counselling Micro Skills. To begin with, let us understand the principles of Counselling. Inform the participants that now, with the help of a few exercises, we will move towards understanding the principles of counselling.

Rapid Fire Round
(Skip this activity in two-day trainings)

- ➔ The Facilitator will stand in the centre of the room and ask all the participants to stand in one or two lines facing the Facilitators. Facilitator will give following instructions:
- ➔ I will read out and present some statements.
- ➔ Listen to the statement and if you ‘Agree’ stand to my RIGHT and if you ‘Disagree’ stand to my LEFT. You will have to instantly decide. If you are in a doubt while responding to any of the statements, please select one of the two options that you feel relatively closer to.
- ➔ After the instructions, the Facilitator will read aloud each statement from the list. Facilitator will pause only for five seconds after each statement, while the participants move to the left or right.
- ➔ The Facilitator will ask each group on both sides to justify their stand and correct any myths or misconceptions narrated by the groups.
- ➔ Allow the participants to rethink their positions and to change sides if they wish.
- ➔ Ask the participants to regroup in the centre of the room after a brief discussion on each statement and participants will have taken sides firmly.
Statements:
Link for Hindi translation of statements
https://drive.geogle.com/drive/folders/13gbs6nvm7hYifvDFUhvCUZKnfep7zs2Y
- Having a TB Patient brings shame to the family.
- It is difficult for a TB Patient to get married.
- It is necessary to have a separate ward for TB Patients in every hospital.
- Patients do not listen unless they are scolded.
- There is a risk of getting TB infection if one visits a TB Patient’s home.
- Patients are so lazy; they don’t even come to the Primary Health Centre to collect their medicines.
Conclude the activity by discussing the key points given below.
Key points to emphasise:
- Tell the Participants that this exercise was meant to make them aware of their own attitudes and beliefs as an individual and bring out one’s attitudes openly.
- The exercise helps to understand that one may respond to a situation in a certain way in one’s personal life, but similar response may not necessarily be desirable and appropriate in a professional setting and in the context of professional ethics.

Understanding Principles of Counselling

Inform the participants that we will now undertake an activity to understand the principles of counselling.
Divide the participants into 4 groups. This could be done by asking participants to stand in a row and say Apple, Mango, Orange and Grape one after the other. Ask everyone who said of Apple to form one group, Mango the second group and so on.
Give each group a cutout of a human shape (Refer to the picture in the Annexure} and ask the groups to write the principles they feel are important for the counselling process.
Inform the group that they need to appoint one leader who will facilitate the discussion, write the points and also present them. They will get 5 minutes to discuss and 2 minutes per group to present.
You can add that it is ok if they do not know the correct terms for the principles, they can just describe them.
When the group leader is presenting, Facilitator will appreciate the efforts of the group and pick up only the principles and write them on the board and say that we got these principles form this group.
➔ After the presentations by all four groups, inform the participants that they have listed several things about counselling. Out of these, some are qualities of Counsellors, some are skills of Counsellors, some speak of the processes or stages in counsellings and some are principles of counselling.
➔ Highlight the principles and say that the skills/processes will be discussed in the next session.
➔ Inform them that you have written only principles of counselling. Like all professions, the counselling profession is also guided by certain principles. These principles are non-negotiable.
➔ Walk the participants through the principles of counselling in the order given in the box. While doing so elaborate on each principle by giving relevant examples.
Alternative:
Facilitator can divide participants into four groups and ask them to choose one of the 4 chits. On each chit will be written one Principle of Counselling (except for last two principles). Each group is expected to discuss and demonstrate the principle verbally or by action without mentioning the name of the principle given to them. Others will have to recognize the principle being demonstrated. After all 4 principles are demonstrated, correctly recognised, and discussed, Facilitator will write remaining 2 principles on the board viz. Autonomy/Self-determination and Beneficence and Non- Maleficence and explain them to the participants.
- Justice and Non-Judgemental attitude: Being fair to every patient. Not having. prejudice or bias against any patient.
- Acceptance: Accepting the clients/patients as they are. Not to have any preconceived notions based on any criteria like background, the appearance of the patient, etc.
- Confidentiality: Not sharing their personal information with anyone else.
- Controlled emotional involvement: Being sensitive and concerned towards the patients helps to understand their problems. However, being overly emotional would mean not being able to think clearly to support the patient and may lead to mental health issues for the counsellor. Not getting emotionally or physically involved in the patient will ensure the professional boundaries.
- Autonomy/ Self-determination: Patients have a right to take decisions for themselves. Counsellors cannot take a decision on their behalf. Counsellor has to follow this principle while addressing issues related to stigma and discrimination, violence, family problems, financial problems, etc., except for decisions related to medical treatment.
- Beneficence and Non-Maleficence: Working in the best interest of the patient and no harm is done to the patient.
Key points to emphasise:
- Counsellor/NTEP staff undertaking counselling need to have an appropriate attitude and follow the principles of counselling as these can affect the counselling process. E.g., believing that ‘Patients are lazy’ or ‘Patients need scolding’ does not follow the principles of Non-judgemental attitude, acceptance and right to self determination. Therefore, we have to be constantly aware of our attitudes and keep working on them for effective counselling.
- It is easy to understand the principles but can be challenging to follow them in our daily practice.
- Following the principles needs ongoing practice.
- In the flow of things and given the high load of work, we might move away from the principles. But it is important for us to self-reflect and consciously bring ourselves back to them.
- Difficulties and conflicts in following the principles need to be addressed through consultation with experienced Counsellors.
Questions on Introduction to Counselling and Principles of Counselling

- Select the appropriate option from the statements below:
i. Counsellor can share the personal information of TB Patients with others.
ii. Counselling is a casual conversation.
iii. Counselling is similar to giving advice.
iv. Counsellor should not have prejudice or bias against any Patient. - A Counsellor can make decisions for the TB Patient.
i. Correct
ii. Incorrect
Annexure:
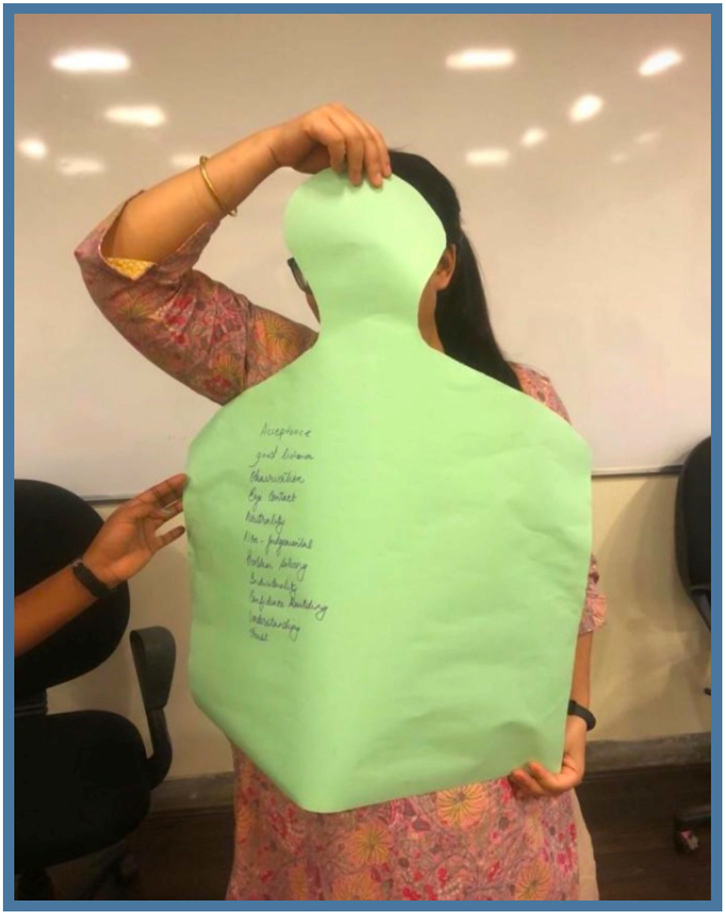
Human shaped cut out used in the activity: Understanding Principles of Counselling
Link for the Handouts on Introduction to Counselling and Principles of Counselling https://drive.google.com/drive/folders/13gbs6nvm7hYifvD FU hvCUZKnfep7zs2Y
Stages and Process
of Counselling


Session Highlights:
Session Overview
Stages and Steps in TB Counselling- Activity 1
Session Recap and Key messages
Session Overview:

In the previous session, part1c1pants learned about the meaning and concept of counselling. They also learned why counselling is important for TB Patients. The session facilitated their understanding of ethics and principles of counselling and provided them with an opportunity to explore personal values and attitudes. Present session aims to take the participants to the next level, by making them familiar with the stages and steps in the process of counselling. The session will also discuss the importance of these stages and steps in counselling by giving the participants an opportunity to practically experience the importance of processes. Master Trainer required for this session: Faculty of Social Work/Ex-Saksham Master Trainers /Prerak Staff/Faculty of Psychology/CBC. Master Trainer who has some experience of practicing counselling will be required. Ideally, the session ‘Introduction to Counselling and Principles of Counselling’, present session and the session ‘Counselling Micro-Skills’ should be conducted by the same Master Trainer or a pair of Master Trainers.
Session Objectives

By the end of this session, participants will be able to:
Define stages and steps in the counselling process.
Understand the pre-requisites (pre-preparation/requirements) of counselling.
Practice the stages and steps involved in the counselling process.
Understand the importance of the various stages and steps.
Time allowed
1 hour 30 minutes
Material required

IJ Electric Kettle/Induction
IJ Tea Bag/Tea leaves/Tea Dust/different types of tea
IJ Tulsi leaves/Ginger/Lemongrass/cinnamon/elaichi /black pepper (additional but desirable}
IJ Sugar/Jaggery/Brown Sugar
IJ Milk/Milk powder
IJ Container to make tea
1J Water
IJ Cup
IJ Strainer
IJ Snacks (additional}
IJ Tray (additional}
IJ Chart Paper
IJ Pen/pencil/sketch pens
IJ White board marker
IJ Copies of Handouts (Annexure l} for the participants/ Soft copies
Method
Preparation before the session:
You as a Facilitator will –
Keep the above-mentioned items ready in advance and keep them at a place in or outside the training hall where they can be easily operated.
As a Facilitator make sure that the arrangement should be in a way that four people can make tea separately at the same time.
Keep as many items as you can so that different kinds of tea could be made.

Chai-pe- Charcha!
(Discussion over tea)

Divide the participants into four groups of equal numbers and invite one participant from each group as a volunteer.

Tea Making (15 minutes)
These 4 volunteers will be asked to make Tea for the participants of the group assigned to them.
Tell the volunteers that the material is laid out and they are free to make the tea, whichever way they like. However, all four volunteer participants must make separate tea as per the number of group members.
Facilitators can be part of any one group.
When tea is being prepared by four volunteers, Facilitator needs to keep members of all groups involved in some activity. It can be feedback from each participant on the sessions so far or sharing the happiest moment in their lives.
Chai-pe Charcha /Discussion (10 minutes)
The volunteers will serve the tea to their respective groups. All members of the group including the volunteer can sit in a circle and enjoy the tea.
There will be four such tea circles.
Tea Story (20 minutes)
After, noting down the stages and steps two members from each group will make a presentation on:
- The detailed Process of tea making as described by their Tea volunteer to them (including the stages/steps followed)
- Their feedback about tea (there can be different opinions of the members about the tea- some may have liked it some may not have liked it, hence present all the opinions)
- What were the things which made their tea unique/special/not up to the mark?
- Anything new about tea making which you learned from your volunteer. (Each group will get 5 minutes for the presentation)
Tea and Counselling (30 Minutes)
As a Facilitator, you will –
Discuss how the process of Counselling is similar to tea-making or anything we prepare in our kitchen. There is an aim to what you are doing, in this instance, the expected outcome was that the tea must be made and presented in such a manner that it tastes best to the person you are making it for. You will not insist that someone with diabetes have tea with sugar, and if you do, that means your tea making has not achieved its objective. It rather caused harm (maleficence) to the person instead of benefitting them (beneficence).
In the above activity, where you presented the steps in tea making by your volunteer, we could understand that not all teas were the same, but everyone was successful in making the “Tea” in their own way.
Here Facilitators would ask participants how do they think this is related to counselling
There were volunteers who asked their group members what type of tea they would prefer while there were others who made it according to their own choice. It can be related to the fact that “counselling is an Art” and “Every Individual is Unique”, hence even though the objective of counselling is the same i.e., “betterment of the Patient”, we cannot decide on behalf of the Patient. Hence, we need to assess the Patient and find out what suits them best.
Because it tastes best, we cannot impose ‘Tea with sugar’, onto a Patient who has diabetes or “Tea with milk” to a Patient who is lactose (dairy products)-intolerant. Similarly, we cannot advice someone on the basis of what we feel is good or best. Therefore, in counselling, even though our objectives can be the same, they are personalised as per the Patient’s situation. For example, asking Patients below the poverty line to include eggs in their diet and a person with high socio-economic status to include protein powder and nuts, to make the unique plan with the same objective to fulfil the nutritional need of both.
Therefore, the “Counselling Process” and process of “Tea Making” can be understood in three stages:
- Stage 1: Setting up the pre-requisites
a) Acquiring appropriate knowledge and information
b) Procuring the material
c) Keeping the material ready - Stage 2: Applying the process/Counselling process
a) Establishing relationship
b) Gathering information
c) Tailoring information
d) Setting a goal on basis of the information received and shared
e) Working on the goal - Stage 3: Feedback/Follow up/Termination
a) Summarisation and Feedback
b) Follow-up
c) Referral to other services/professionals such as social worker, Doctor, legal services etc.
d) Termination if the goal is achieved
Conclusion (10 Minutes)
Facilitators will conclude the session by saying that – In the previous session we saw what Counselling is and what are the principles of counselling. In this session, we saw the stages and steps of counselling. While counselling Patients there are different approaches. We are going to discuss such approaches in Counselling.
Currently, the most widely used approach is the GATHER approach. While counselling a Patient we should follow a step-by-step process. GATHER is an acronym that will help you remember the 6 basic steps. It is important to know that not every new Patient needs all the steps – you need to use the GATHER approach sensitively so that it is appropriate to each Patient’s need. You may need to give more attention to one step than the other.
GATHER is an acronym:
- G stands for Greet the Patient respectfully
- -A stands for Ask them about their needs
- T stands for Telling them different options available to address their problem
- H stands for Helping them make decisions
- E stands for Explain and demonstrate
- R stands for Return/Refer; schedule and carry out a return visit and follow up
It is important to give more emphasis to the points under each counselling step.
The second approach that is also being followed is REDI approach.
REDI: A Client-centred Counselling Framework.
REDI is an acronym:
- R stands for Rapport Building
- E stands for Exploring
- D stands for Decision Making
- I stands for Implementing the Decision
REDI framework emphasises the client’s perspective and empowers health professionals to better enable new and returning clients make full, free and informed decisions. For new clients, REDI emphasizes the importance of helping clients select the option that is best suited to their unique situation.
Both GATHER and REDI approaches have been documented as effective while counselling on family planning or helping Patient select a correct contraceptive method.
Key points to emphasise:
- Counselling is an Art like tea making. It is a process. There are some common stages and steps in both, yet both require innovations and skills based on who we are providing it to.
- It is important to assess the Patient and understand their situation/social reality before applying ready-made counselling steps to them as you can’t serve tea with sugar to a person with diabetes, no matter how better it tastes with sugar. Hence, Counselling has to be need-based – i.e. Patient- centric.
- There are three important stages of counselling. Setting up the pre- requisites, Applying the processes/ Counselling process, Feedback/ Follow up/Termination. Each stage has steps to be followed.
- There is flexibility in steps and skills you use depending on who you are providing the counselling to, but there are some important pre-requisites. For example, you cannot make tea if you do not have basic knowledge of making tea, have tea in any form, water/milk, container to make it and something to heat and then a medium to serve it, like a cup.
- Similarly, the pre-requisite for counselling is to have correct and updated knowledge in the area, history-taking form, pen/ pencil, referral list, information material, empathy, non-judgemental attitude, respect, and commitment to Patient’s welfare are must for counselling.
Questions on Stages and Process of Counselling

- _____________is the first stage of counselling process.
i. TB Treatment Education
ii. Rapport building
iii. Giving advice - When can a Counsellor terminate the TB Patient counselling?
i. After treatment initiation
ii. Beginning of the Continuation Phase (CP)
iii. Treatment Completion
Handout : Art of Tea Making and Counselling
Handout : Art of Tea Making and Counselling
Link for the Handouts on Stages and Process of Counselling -Art of Tea Making and Counselling https://drive.google.com/drive/folders/1fPG2dBcSdVKbjOIdoY4ifK5EgDYESmrq
| Stages | Tea Making | Counselling |
|---|---|---|
| Stage 1: Setting up the pre-requisites a) Acquiring appropriate knowledge and information b) Procuring the material c) Keeping the material ready | You keep the material ready; Tea bags/leaves, sugar, milk, stove, water, container, induction/gas stove to cook, extra ingredients, cups to serve. You also consider for whom are you making the tea. Your partner may like it strong, but your child prefers it with ginger and Tulsi leaves. And the neighbours you invited may like jaggery instead of sugar. Hence, accordingly you keep the material ready. Here you may not be knowing (first time) or may be knowing (follow-up session) that what another person may like. | You keep your set-up ready- pen/pencil; forms to be filled, information brochure to be given, referral contact no’s/form, Questions to be asked to collect the history of the Patient. Link for the Handouts on Stages and Process of Counselling -Art of Tea Making and Counselling https://drive.google.com/drive/folders/lfPG2dBcSdVKbjOldoY4ifKSEgDYESm |
| Stage 2: Applying processes/Counselling process a) Establishing the relationship/R apport Building b) Gathering information c) Giving information d) Setting goals on the basis of received and shared e) working on the Goal | a) You gather everything together. Keep the container on the stove, light it/Switch on the Induction b) You ask them what type of tea they would like to have c) You tell them what ingredients are available with you, green tea, Taj Tea, Tata Tea, Tea bags, ginger, Lemon, cinnamon …. d) On basis of what they tell you and the and ingredients available,you decide to put them to use and make the tea e) Finally, the tea is ready, and you serve it. To serve it you use the cup best suited for the one you are giving the tea to.E.g, for children you would not prefer glass cups. Tea is served and enjoyed. | a) You make the Patient comfortable by building rapport with them. So that they are not hesitant in sharing information with you and you can ask the required questions. Towards this you use some skills and share some information with them so that they trust you such as: l.You introduce yourself 2. You ask for their introduction. You tell them about confidentiality. You maintain Privacy and explain to them the services available at the centre. b) You ask them about their concerns if they do not talk about it explicitly, you try to assess them using micro skills. c) You give them correct and updated knowledge. Tell about the services available in the centre d) On the basis of the information received and the available options. you ask the Patients to choose the one which works best for them. You devise the ways for them to implement, for example; A Patient who forgets taking regular medicine gives options that while watching a certain TV series he will take the medication and, in the morning, when milk is delivered, he would take the medicine. The plan is ready. e) The Goal is achieved here as all medicines are taken regularly without missing a single dose with all nutritional supplements and all prevention modes are adopted |
| Stage 3: Feedback/ Follow up/ Termination Summarisati on and Feedback Follow-up Referral to other services/prof essionals such as social worker, Doctor, legal services etc. Termination if the goal is achieved | a) Summarise and ask how the tea was and you can also assess if the whole tea was consumed or some of it was left it. Have they asked for another cup of tea? b) You invite them again at another time. c) You can now talk about other options which you do not have but they can enjoy from other sources like a specific type of green tea/coffee. d) They can make a similar tea now on their own | You briefly talk about the important points in your session so that you can make sure that Patient has understood them in the same manner as you wanted to convey. The Patient shows consistency in following up on the plan and showing improvements. You decide on follow-up session to ensure that the plan is consistently followed. In case you feel there is another service required by the Patient, such as legal service, nutritional support etc., then you refer the Patient to that service. On successful completion of treatment, you close the session as your goal is achieved. |
Stages in Counselling Process
Stages in Counselling Process
Stage 1: Setting up the pre-requisites
Stage 2: Applying the process/Counselling process
Stage 3: Feedback/ Follow Up/ Termination
Counselling Micro-Skill
Counselling
Micro-Skill


Session Highlights:
Session Overview
Activity 1 – Meaning and Introduction to the counselling Micro-skills
Activity 1 a – Walk a mile in my shoes
Activity 2 – Practicing the skills…Hum Honge Kamayaab
Session recap and Key messages
Session Overview:

In the previous session, we went through the various stages and steps involved in the counselling process. It was explained using example of tea making and how the steps in counselling and teamaking are comparable. The present session goes beyond the stages and steps and introduces various micro- skills which are essential and helpful in effective counselling. The session aims to introduce these micro-skills and provides an opportunity to practice these skills.
Master Trainer required for this session: Faculty of Social Work/ Ex-Saksham MTs / Preak Staff/ Faculty of Psychology/ CBC. Master Trainer who has some counselling practice experience will be required. Ideally, the session on ‘Introduction to Counselling and Principles of Counselling’, the session on ‘Stages and Process of Counselling’ and this session should be conducted by the same MT or a pair of MTs.
Session Objectives

By the end of this session, participants will be able to:
Enumerate Counselling Micro-Skills.
Familiarize themselves with the skills
Time allowed
2 hour 15 minutes
Material required

IJ Printout of Annexure l for Facilitators for Activity l
IJ Dance beat song (Hum Honge Kaamyaab and amplifier/speakers for Activity 2
IJ Chits of Case study from Annexure 2 for Activity 2
IJ Small Basket/bowl and any object which can be used as a parcel for Activity 2
IJ Whiteboard marker
Method

Meaning and introduction to the Counselling Skills

As a Facilitator you will –
Introduce the session by saying that – ‘In the last session we learned the steps and process of counselling, hence, now we are aware of “what is to be done” in a counselling session beginning with “rapport building till the termination of the session and referrals and networking. Now, it is known what to do but “how it is to be done” is the question which remains. The current session addresses these questions.’
The answer to the above question is “skills”, which are a set of verbal and non verbal tools a Counsellor/NTEP Staff must have to conduct an effective session and meet the set objectives. In the tea session we knew that the objective was to “make tea” but how to make the tea was the “skill set”- how much water to boiled, when to add the ingredients, how much sugar would be required, whether the milk is required or not… all these explain the skills required for tea making. Hence, with the required knowledge anyone can make tea but not all would be able to make a “good Tea”. The one who has the appropriate skills would only master it, which means skills can be learned. Similarly, by learning about counselling all participants can conduct counselling, but to have a “good counselling session”, some skills are required. These skills can be known as “Micro-skills”, which are essential for effective communication and development of a supportive Patient-Counsellors/NTEP Staff relationship.
Tell them that they have already been doing the counselling. They must be doing all steps of counselling properly, steps l, 2, 3 and so on…. But these micro-skills work at the level of 0.5 steps, i.e between the steps. If they skip these 0.5 steps, while counselling, it may not be effective. On the contrary, if they make conscious efforts to include them while counselling, their counselling will be more effective.
Conclude the discussion by explaining each counselling micro skill, except Empathy, on the board with keywords/key statements to be used while demonstrating the skills. (See the table below). Some participants might take photo of the board for their reference. Also, reassure them that the PPT and handout will be shared with them on the WhatsApp group after the training.
| Micro Skill | Keywords /statements to be remembered/used |
|---|---|
| Leading Question (Remember not to use it in counseling at all) | Sentences with question tags, like – right? isn’t it? correct? na? and the leading tone is indicative of the leading question. For example – You are taking medicine regularly, na? Instead of asking the question in this manner try asking such questions in a neutral tone or change it to open such as ‘Are you taking medicines regularly? Or ‘How are you taking medicines? One can use words such as ‘what, how, how come, who, from where, when etc. |
| Open-ended Question | Asking the Patients to express more, beyond one or two words. Ensuring that the questions to be asked should not be closed-ended i.e. can not be answered only by ‘Yes’ or ‘No’. For e.g. Closed-ended question – Did you eat, today? Open-ended question – What did you eat, today? |
| Clarification | Ask for further information for more clarity by saying – Can you please elaborate? Can you please explain? |
| Reflection | Hint is how Amitabh Bachchan reflects in Kaun Banega Crorepati. Try to understand the feeling expressed verbally or non-verbally by the Patient and say – Are you (name of the feeling/emotion)? Such as- Are you tense? Are you confused? Are you anxious? etc. |
| Paraphrasing | Remember that Paraphrasing is done only by the Counsellor. It is restating the Patient’s words in a shortened and clarified form and thus ensuring that their words are in congruence with the Patient’s verbal and non-verbal language. Say – According to you, ……., Do you |
| Summarisation | Remember narrating story of the movie Sholay in 5 lines. Counsellor can summarise at the beginning of session to recap the previous session, or in-between present session while concluding the previous discussion and moving to next topic of discussion or at the end of every session to recap what was discussed in today’s session. Counsellor can say – Here/At the end of today’s session I would like to summarize that-……………. It is not mandatory that only Counsellor should summarise. Rather, Counsellor can request the Patient to summarise at any point by saying – Can you please summarize/tell me in short what did we discussed so far? /Today?/ Last time? |
| Sympathy is to be avoided in counselling | Do not use words such as Arere….Oh ho So sad……Bechara…..Oh …Poor guy etc. These words are indicative of pity/sympathy. |
| Empathy | Always replace sympathy with empathy. Demonstrate empathy by saying I can understand……../This must be very painful/disturbing/ bothering you. |
Tip to the Facilitators

Facilitators have to keep in mind that this part of the session is theoretical and hence, some might lose interest after some time. Facilitators will have to make this session interactive, by asking them questions in between, giving them real-life examples, using humour, sharing personal experiences in lighter vein. A bio-break or tea-break can be allowed, as per the schedule. Assure them that although this is the technical information, things will be clear to them once they practice these skills in the forthcoming activities.


Walk a mile in my shoes

As a Facilitator, you will –
Inform the participants that we will now undertake another activity.
Divide the participants into two groups. Ask one participant to say “In” and the second participant to say “Out”, repeat this.
Ask all “Insiders” to stay in the training hall and the “Out” to wait outside.
Outside the training hall give following task to the “Out”. Tell them that this task is about the Time-Management where they have will to take signatures from each and every “In” within 2 minutes. Ask them to keep a single empty page and pen ready and wait outside. Tell them that the task will start only when you ask them to enter the training hall and they have to stop as the Facilitator says ‘STOP’ aloud. When they are asked, each one them is supposed to count and tell the total number of signatures they have got.
Enter the training hall and in a quieter voice inform the “In” of the task you have given “Out”. However, the task of the “In” is to not give their signatures.
Each “In” will decide one excuse for not giving the signature such as- it’s lunch-time, get the signature from “that” person first, fill form 6 first, there are no pens and hence signatures can’t be given, I am just a peon, the concerned person is on leave, so on and so forth.
Each “In” has to have a specific excuse for not giving a signature.
Also, inform the “In” that their tone has to be extremely rude and they need to create panic as well as a hostile environment for “Out”.
Now ask the “Out” to enter and begin their task.
Let this continue for 2 minutes. You as the Facilitator need to intervene if the “In” are not being rude or giving the signatures.
After 2 minutes stop the task and ask everybody to regroup.
Now ask the “Out” how many signatures each one has got. When everyone from “Out” will laugh and say no one gave them signatures, ask them how they felt. Make a note of their feelings.
Ask the larger group why was this activity undertaken. Most of the participants will be able to identify that this is what Patients go through when they have to navigate treatment in an unfamiliar environment.
If not/even if they do, conclude the activity by stating that this activity was not about Time-Management but it was done to ‘walk a mile in the Patient’s shoes’ and experience their struggles. The Patients are dealing with multiple issues- accepting the diagnosis, concerns about the outcome, dealing with the paperwork, navigating through unfamiliar and sometimes huge health facilities etc.
To understand it better, Facilitator will invite four volunteers from the participants. Facilitator will ask these four volunteers to form a circle and put a sheet of paper with the number 3 written on it. Ask each one to read what they can see on the paper. One person may say 3 whereas the person standing opposite will read it as E. Similarly, the person standing on the other end may say Mand the person standing opposite may read it as W. Now ask any person to convince the person standing opposite to him that what he sees is right without touching or rotating the paper. Do the same thing to the other remaining pair of participants. One of participants may say that the other person will have to come to their position to see the way they look at it. Then the Facilitator can show the paper to all and say, how each one of them was correct. Facilitator can conclude by saying that you can not force the other person to perceive things the way you see it. To understand other person’s point of view, you will have to go to that person’s position. Only then you will understand what the person is trying to say and why.
Assure the participants that all of them are excellent workers but at times due to our processes, high Patient load, reporting stress and personal worries we all tend to disconnect from the feelings/struggles of the Patients.
We need to be aware of this and consciously make efforts at empathising with our Patients. We can keep a jar on our desk and drop a pebble in it every time we lose our cool, make a note of what was the trigger and try to work on it.
Encourage the participants and tell them that you are confident that with awareness and practice the jar will slowly and surely remain empty.
Tip to the Facilitators

This activity has to be conducted in an absolutely sensitive manner. Care needs to be taken to ensure that the participants don’t feel judged and blamed. As Facilitators you need to empathise with the participants. A personal experience from the Facilitator’s own professional journey will help

Spotlight – Skills Practice….. Hum Honge Kaamyaab…….

Print Annexure 2, cut individual situations along with the skill for demonstration and put them in a small basket.
Facilitators will request the participants to sit in circle.
Facilitators will explain the activity by saying – This activity has to be played like the ‘passing the parcel activity’ i.e. music has to be played, a small parcel, such as a ball, has to be passed amongst the participants who will be playing the role of the Counsellor in this activity. The person who has the ball in hand when the music stops has to pick up one chit from the basket. Ask the participant to read out the situation and the skill to be demonstrated mentioned below the situation. Each participant will be given only 2 minutes to demonstrate the skill as a Counsellor/ NTEP Staff. For each situation, Facilitator can play the role of the Patient as described in the chit. Alternatively, Facilitator can ask the participant who acted as a Consellor in one case to be the Patient in the next case. Facilitators will ensure that the demonstration of the skill through the role-play is easily visible to the rest of the participants.
After the participant has demonstrated the skill, the Facilitator will ask the other participants for feedback.
Facilitators will ask the other participants to demonstrate the same skill, if more clarity or practice is required.
Please ensure that the participants are focusing on the skill mentioned in the chit only and not getting into counselling or “problem-solving”. Bring back the demonstration to practicing the skill.
Key Learnings:
l. “Skills” are a set of verbal and non-verbal tools which a Counsellor/NTEP Staff must have to achieve an effective Counselling session and meet the set objectives.
2. Respect , acceptance , non-judgmental attitude and empathy are essential counselling skills for Counsellors/NTEP Staff which can be achieved through active listening, mature responding, clear and updated knowledge/ information sharing.
3. The role of non-verbal communication is equally important as it validates the verbal skills.
Questions on Micro-Skills in Counselling

1} __________is to be avoided in counselling.
i. Sympathy
ii. Empathy
iii. Reflection
2} _____________cabnedone by the Patient.
i. Paraphrasing
ii. Summarisation
Annexure 1
Handout: List of skills with Description and Demonstration
Handout: List of skills with Description and Demonstration
Link for the Handouts on Counselling Micro Skills
https://drive.geogle.com/drive/folders/ltj37sjrFxtmnP35M 8fXZsy80EGFZfLhA
| Micro- Skill | Description of the micro-skill | Demonstration of the particular micro-skill |
|---|---|---|
| Rapport Building | ||
| Rapport Building | Establishing an interpersonal relationship or rapport is the foremost step to initiate any counselling session. Subsequent counselling stages are likely to be more effective if Counsellors/NTEP Staff first establish a good rapport with the Patient. There are certain factors which facilitate establishing the required relationship between the Counsellors/NTEP Staff and the Patient. Following is the detailed description of the skills which help in rapport building: | |
| Greeting the Patients and Introducing Self | Counsellor/NTEP Staff tells the Patient their name, a brief description about the centre and its functions and the Counsellor’s/NTEP Staff’s role in that particular centre. | As the Patient enters the room – “Namaste! I am ABC, appointed as a TB Counsellor/NTEP Staff in this centre. This centre primarily aims at providing TB prevention and treatment management related counselling and testing services free of cost. Considering the sensitivity of the TB testing and related concerns, all information shared between you and me along with the test. results will confidential”. |
| Using Silence | ||
| Using Silence | Silence can be used in various situations – In the course of counselling, Counsellor/NTEP Staff is supposed to show patience until the Patient is able to provide additional input and responds further It is important for the Counsellor/NTEP Staff to allow the Patient to gather thoughts and regain composure. Patients get the space to experience feelings during silence. While going through intense emotions patients cannot absorb much information. Silence can be used in such situation | The Counsellor/NTEP Staff either pauses or remains quiet for a few minutes, after asking the Patient certain questions that require the Patient to share their personal experiences,feelings or thoughts. The Counsellor/NTEP Staff uses statements like “You can take your time” During this time, the Counsellor/ NTEP Staff appears Patient and makes eye contact with the Patient. The Counsellor/NTEP Staff does not fidget or appear uncomfortable. The Counsellor/NTEP Staff does not allow the silence to continue for very long {avoiding discomfort and awkwardness). |
| Active Listening | ||
| Listening and Active Listening | Counsellor/NTEP Staff need to be excellent listeners. Further, active listening is one of the important skills during counselling. The Counsellor/NTEP Staff needs to pay full attention to what the Patient says {verbal- linguistic communication), how the Patient says it {verbal- paralinguistic communication) and what the Patient seems to be feeling {based on nonverbal communication). All of this help to convey the Patient’s total message. The Counsellor/NTEP Staff listens for total meaning i.e., focuses both on the content and the feeling or attitude underlying the content and responds appropriately and sensitively to the Patient. Thus, listening to what is said and also listening to what is not said. The Counsellor/NTEP Staff is aware that not all communication is verbal and that a Patient’s words alone do not tell us everything that they are communicating. As much as 70-80% of our communication is non- verbal, i.e., expressed through body language such as facial expressions, body posture, hand movements, eye movements and breathing. In addition, verbal communication is of two types – linguistic and paralinguistic. Linguistic communication is simply- all the words we utter. Paralinguistic communication is the way we speak- including the tone, volume, speed of speech, pauses and sighing while we speak. Thus, any set of words, e.g., “I am okay”, or “Yes, I am taking the medicines” may mean different things depending upon the way we say them. | Patient: “I told my FAMILY that I have TB. They are afraid that now I will transmit it to other family members. They are not even giving me a glass of water”. Counsellor/NTEP Staff: “I understand that you felt bad about this behaviour of your family members. We can explain to them in detail about transmission and prevention of TB”. |
| Questioning | ||
| 1. Closed ended 2. Open ended 3. Leading | For effective counselling it is important to use a mix of open and closed- ended questions. The Counsellor/NTEP Staff does not use closed-ended questions in quick succession, as the Patient may feel being interrogated and will become defensive. The Counsellor/NTEP Staff combines open- ended questions with a few closed ended questions to allow them to decide direction in which they want to take the conversation. The Counsellor/NTEP Staff uses adequate closed-ended questions to collect facts pertaining to the Patient’s problem as well as the basic details like the Patient’s name, age and marital status, where does the Patient reside and information about the Patient’s family members. As the session progresses, the Counsellor/NTEP staff begins to use more open- ended questions. These questions seek out the Patient’s thoughts, emotions and experiences and invite the Patient to continue talking and sharing emotions Leading questions by the Counsellor/NTEP Staff unwittingly suggest answers to unwittingly suggest answers to will not give the Counsellor/NTEP Staff a correct picture of the situation. Therefore, avoid using leading questions. | Open-ended questions: An open-ended question requires more than a one-word answer, e.g. “What difficulties do you experience in following regular DOTS?” “How do you think you would manage your routine so that it ensures complete treatment?” “When do you think would be a convenient time for you to come to the centre?” These cannot be answered by a simple ‘Yes’ or ‘No’ or any other one or two words. These questions invite the Patient to continue talking and help the Counsellor /NTEP Staff decide the direction of the conversation. Closed-ended questions: A closed-ended question limits the response of the Patient to one/few word answers, e.g. -“Do you practice behaviours necessary for preventing TB transmission to others?” -“Who allare there in your family?” -“Have you taken the medicines today?” -“Have youhadbreakfast?” Closed- ended questions do not give much opportunity to a Patient to think about what they are saying. • Answers to such questions can be very brief, hence non-informative. This often necessitates further and thoughts. • However please note that closed ended questions are not bad in themselves and will have to be used in certain situations, e.g. -‘Are you experiencing any side effects of the medicines?’ -‘Does your family know that you have TB?’ ‘You have taken the medicines as prescribed, haven’t you?’ ‘Do you agree that you should always adhere to the treatment?’ “You don’t have any ADR, right? |
| Reflection | ||
| The Counsellor/NTEP Staff is accurate in recognising the emotions that lie beneath the Patient’s verbal and non- verbal communication. The Counsellor/ NTEP Staff reflects back to the Patient with the useof a different set of words, the emotions that the Patient seems to be feeling. In the column at the right, the feeling words have been underlined, to illustrate that the Counsellor/NTEP Staff needs to accurately identify what the Patient is feeling. | Patient: “Is my wife all right? Are there any complications? I just don’t know what is going to happen?” Counsellor/NTEP Staff: “It seems like you are anxious about your wife’s health…!” | |
| Clarification | ||
| is very important to clarify and t assume on behalf of the tients. The Counsellor/NTEP aff asks the Patient appropriate estions about the information ared by the Patient. Questions seek clarification are often rded differently than the ening question asked by the unsellor/NTEP Staff. | Patient: “I am taking medicines regularly for three weeks, but I think it is of no use.” Counsellor/NTEP Staff: “OK. Can you please elaborate more on ‘it did not work…’ as I did not get what you mean? | |
| Paraphrasing | ||
| The Counsellor/NTEP Staff restates or repeats the Patient’s words in a shortened and clarified form. While doing so, the Counsellor/NTEP Staff ensure that their words are in congruence with the Patient’s verbal and non- verbal language This is called Paraphrasing. It is important to note that Paraphrasing is not repetition. Also, the Counsellor/NTEP Staff can use some of their own words to convey the real meaning of what the Patient may be saying. | Patient: “My wife irritates me. She picks on me for no reason at all. We do not like each other.” Counsellor/NTEP Staff: “So, what you are saying is that you are having problems getting along with your wife. You are concerned about your relationship with her.” | |
| Summarising | ||
| Summarising lets the Patient know that the Counsellor/NTEP Staff has heard and understood and. It also enables the Patient to clarify thoughts, identifying what is most important. It is not sufficient just to notice what the Patient has said, it is also important to notice what is missing. Summarising is different from paraphrasing, as a summary usually covers a longer time period than a paraphrase. Thus, summarising may be used after some time: perhaps halfway through or near the end of a counselling session. | Counsellor/NTEP staff: At the end of our session, I would like to summarize that your TB treatment will go on for 18 months…. Or Counsellor/NTEP staff can also ask the Patient to summarize by saying – “Can you tell me what we have discussed today?” | |
| Communication | ||
| Body language (movements) | Non-verbal communication is equally important in counselling and one needs to be aware of one’s own body language during the counselling process. | Non-verbal communication is equally important in appropriate posture i.e., not sitting too close or too far from the Patient. |
| Grooming and appearance Use of touch | The Counsellor/NTEP Staff makes use of hands, head and overall body posture appropriately during the session which makes the Patient feel comfortable. Appropriate clothing which is not flashy is recommended along with a neat and clean look. | Also, Counsellor/NTEP Staff should be sitting straight but slightly leaning forward to demonstrate interest. Counsellor should be wearing appropriate and decent clothes so that the focus of the Patient remains on the session and not on the clothes and the untidy appearance. Use hand movements wherever applicable, nod your head moderately. Sit with open arms, do not sit with your arms folded. (This will denote an accepting stance.) Don’t keep moving your legs or twiddling your fingers (this denotes impatience). As far as possible avoid touching the Patient, especially, when the Patient is of the opposite gender and in TB counselling physical distancing is important. |
| Facial expression | Our face is the route to our inner feelings and concerns. Through our facial expressions, we can convey a lot of feelings, emotions and concerns to the Patient. Through our expressions we can convey that we are listening, we understandand, we require some more information or we are unclear. | Wear a smile on your face whenever a Patient enters the clinic. Use your hand to indicate the place where the Patient should sit. Incline your head towards the Patient while talking to the Patient. If TB Patient is sharing something serious, reflect the same from your facial expressions like lowering your smile, curve and slight nod with the use of “hmmm”, “ok” or silence will work here. |
| Eye contact | Eye contact helps in observing the Patient and facilitates relationship building. Appropriate eye contact makes Patients feel that they are being paid attention to and are being listened to. Similarly, it also gives important information to the Counsellor/ NTEP Staff if the Patient is comfortable, interested or understanding the information. | Look at the Patient appropriately. Do not stare. You may lower your eyes occasionally to make the Patient comfortable. But somewhere else. |
| Empathy | ||
| The Counsellor/NTEP Staff is able to put themselves in the Patient’s situation and understand what the Patient is thinking and feeling. In addition, the Counsellor/NTEP Staff is able to communicate (verbally and non-verbally} with the Patient that the Counsellor/ NTEP Staff has understood what the Patient is thinking and feeling. | Patient – I am so worried; how long do I have to take the medicines? I live alone here. “I can understand how you must be feeling at this moment…l would like to add that I am here for you and will support you during this process” Patient- There are so many medicines, how will I manage this? “I can understand your concern …. I am here for you; I will explain the process of taking the medicines and together we can develop strategies to remembering’ Similar examples can be given whereby the participants clearly understand empathy. | |
Handout: Understanding Counselling Skills and Core Competencies
Handout: Understanding Counselling Skills and Core Competencies

Situations for Skills Demonstration
Annexure 2
Situations for Skills Demonstration
Link for Hindi translation for Situation for Skill Demonstrations
https://drive.geogle.com/d rive/folders/ltj37sjrFxtmnP35M8fXZsy8OEG FZflhA
Patient’s name can be changed suiting to region and culture.
Savitha is a 35 year old married woman. She is on TB treatment for 3 months. You are meeting Savitha today for follow-up Counselling.
Demonstrate the use of 2 open-ended questions and 2 close-ended questions.

Bhaskaran is 62-year-old, retired postman. He has been diagnosed with TB, 2 months ago. Now, he is thinking of going to his village and staying separately there, away from his family.
Demonstrate Paraphrasing done by Counsellor/NTEP Staff.
Focus only on Paraphrasing and not on other counselling points or TB information.

Abha, is a 20 year old college student and has been diagnosed with TB a month ago. She feels that if her friends get to know her status, she might lose them. She has started avoiding them.
Demonstrate Reflection
Focus only on Reflection and not on other counselling points or TB information.

Mary is a 35 year old woman and taking DR-TB treatment for the past 3 months. You are meeting her for follow-up counselling today and during the counselling she shares that she is taking too many medicines due to which she is having unbearable headaches.
Hence, she wants to stop her medicines.
Demonstrate Empathy. Focus only on Empathy and not get into follow-up counselling or TB information.

Sing a song or share a joke.

You have undertaken nutrition counselling for John, who has recently started treatment.
Demonstrate Summarization

Enhancing
Counselling
Competencies for TB


Session Overview:

This session will give an opportunity to the participants to practice the competencies and skills which they learned in the previous session in the context of three important stages of the TB counselling: Initiation, Treatment and follow-up.
Master Trainers required for this session: Ideally a Master Trainer who has Counselling Practice experience and should be the same Resource Person who has conducted the Micro-Skills session.
Session Objectives

By the end of this session, participants will be able to:
Utilise counselling competencies and skills in counselling.
Time allowed
2 hour 30 minutes
Material required

- Chart Paper
- Pen/pencil/sketch pens
- Whiteboard marker
Method
Activity on the next page
Please see the alternative activity at the end of annexure for states where DRTB burden is low and there might be other challenges.

Practising Counselling Competencies and Skills

Preparation one day before the session:
You as a Facilitator –
- Keep 5 cases (Annexure 1) ready with you. For case no. 1, 2 and 3, you will have 3 copies each. For Case no. 4 and 5, you will need 4 copies each. (Soft copies of the cases can also be shared with the participants).
- Divide the participants into 5 groups and ask each group to nominate participants who will perform the role-play. Groups l, 2 and 3 will require 3 participants and groups 4 and 5 will require 4 participants for the role-play.
- Give an appropriate copy of the case study to each participant nominated by their Respective group and ask them to go through the cases given to their groups, discuss and prepare the role-play. The time allotted to prepare is 10 minutes and for performance of the role-play 5 minutes.
- The remaining participants in each group will be responsible to keep the time for the previous group and provide feedback to the Counsellor in the role-play based on the Micro-Skills used or those which could have been used during the role-play. Thus, when group l is performing the role-play, the observers belonging to the second group will keep the time and give feedback after the role-play. Each group will receive feedback from the next group. Group 5 will receive feedback from Group 1.
- Instruct all participants to stick to the role assigned to them. While doing the role play, acting skills will not be judged and the focus will be on the Counselling process and micro-skills used while counselling. Once the role-play is over, participants involved in the role-play are not allowed to speak while feedback is being given by the observers from the next group.
- Facilitators will check and comment on the Process of counselling, principles of counselling, micro-skills used or not used, use of language while counselling, any bias or prejudice seen in the role-play and change in attitude, wherever needed.
- Facilitator will also ensure that the Counsellor has understood and demonstrated what counselling is and what counselling is not, and has not committed errors while counselling (Refer to Key Learnings after activity l, Matters of Heart in Session on Introduction to Counselling and Principles of Counselling).
- Facilitator should also check and discuss if any change in the attitude or perspective is needed. Check if the Counsellor is using any cliche while providing counselling. (Refer to the statements in the session on Our Words Our Perspectives).
- Facilitator can check if Counsellor is giving unwarranted assurances at any point in the counselling. If Counsellor is doing so then Facilitator should help everyone to understand what are the serious implications of unwarranted assurance in counselling, such as loss of trust, questioning by the Patients etc.
- If Facilitator observes that the Counsellor is undermining or denying Patient’s problem or tension in any of the role-plays, then the Facilitator can have all participants close their eyes for 2 minutes and NOT THINK OF ELEPHANT. They can visualize or think about anything but an ELEPHANT. While instructing Facilitator should use the word ‘elephant’ several times. After two minutes Facilitator can ask the participants to open their eyes and report how many of them saw elephants when their eyes were closed. This way, Facilitator can demonstrate how asking the Patients not to worry or not to take tension may either undermine their feelings or will lead to denial of their emotional status. At times, it may lead the to insertion of such feelings or thoughts even if the Patient is not feeling so.
Tip to the Facilitators

This exercise is meant for practicing counselling competencies and skills. Summarise the main learning points from all role-plays.
In case participants do not adhere to the given guidelines, intervene in between the role play and/or presentations.
Try to focus on various skills used during the role-plays by giving specific examples from the role-play such as using questioning, paraphrasing, summarization, reflection of feelings, empathy, non-judgmental attitude etc.
Debrief at the end of the activity.

Questions on Practicing Counselling Competencies

1} Referrals are not allowed in Counselling.
i. True
ii. False
2} Counsellor need not talk about the side effects of the medicines before initiating the treatment.
i. Yes
ii. No
Annexurel
Make singlepage photocopies of all Annexures in advance and distribute them to participants or share the soft copies in the group
Link for Hindi translation of cases for Practicing Counselling Competencies and Skills
and Handouts on Checklist for NTEP Staff and Counsellor
https://drive.google.com/drive/folders/1SqJLOZjjSWUXi3N80Ei6fjtRN85f6mOe
(For the participants who will be performing role-play in each group make 3 copies of cases 1 & 2, 3 and 4 copies of cases 4 & 5)
Patient’s name can be changed suiting to the state, religion or culture.
Case 1:
Jayanti is a 32-year-old, woman who is recently married. She is diagnosed with DR TB and referred to you for counselling. She has visited your DTC with her husband, who is a primary school teacher. They live in a joint family.
Please establish a relationship and provide information about the difference between DS-TB and DR- TB, ADR management and adherence to treatment. Stick only to the role assigned to you.

Case 2:
Background – Jayanti is a 32 year old, woman who is recently married. She is diagnosed with DR-TB and referred to you for counselling. You have already met her husband, who is a primary school teacher. They live in a joint family. Her treatment was initiated 2 months ago.
Today Jayanti and her husband have come to meet you for follow-up counselling. Jayanti informed you that she has just got married and it will be difficult for her to take her medicines regularly. Also, her husband is asking if she should go to her parent’s home till the treatment is completed. But Jayanti is not in favour of going to her parent’s home, as her parents are old. Her husband will have to manage the whole family and hence it will be difficult for them to spend extra money on specific diet.
Please provide Adherence Counselling, provide information about hygiene, Caregiver Counselling and diet counselling and any other important issue which comes up in the case. Please do not go back to make a rapport with the Patient as you have already established a good relationship with the Patient. Do not take the history of the Patient because that too has been done in the first visit. Stick only to the role assigned to you

Case 3:
Background – Jayanti is TB positive and in the first session she informed you that she has just got married and lives in a joint family. Counsellor had told her that all members of her household, regardless of age should be given TPT after ruling out TB. Her mother-in- law is found eligible for TPT after assessment.
Today, Jayanti and her mother-in-law have come to meet you for follow-up counselling. Her mother-in-law is a diabetic and is suffering from blood pressure. However, she is not willing to initiate the TPT, as she feels that she is not a TB Patient and her reports are also normal. She further blames Jayanti that it is because of her she has to undergo testing and treatment.
Please provide TPT Counselling to Jayanti’s mother-in-law. Explain to her about eligibility and key messages. Check with her what is the best approach to support treatment adherence. Give her information regarding most suitable location for drug intake and treatment support, explain to her the disease process and importance of completing TPT, discuss possible side-effects and their management. Also, discuss the need for self-monitoring and reporting

Case 4:
Background – Jayanti is TB positive and in the last session she informed you that she has recently got married and it will be difficult for her to take medicines regularly. Also, her husband says if she can go to her parent’s home till the treatment is completed. But Jayanti says, she is not in favour of going to her parent’s place, as her parents are old. Her husband will have to manage the whole family and hence it will be difficult for them to spend extra money on specific diet. In the last session, you have done adherence and nutritional counselling.
Today she has come for a follow-up session along with her mother-in-law and husband. Her family discusses with you about planning a baby as they have been married for more than a year and relatives are putting pressure on them. However, her TB status cannot be revealed to their relatives. The husband also shares that because of TB their neighbours have stopped visiting their home.
Please counsel her for reiterating adherence, hygiene and caregiver counselling along with stigma, discrimination, issues related to family planning and reproductive health and any other important issue which comes up in the case.

Case 5:
Background – Jayanti is TB positive and in the last session she came along with her mother-in-law and husband. Her family discusses with you about planning a baby as they have been married for more than a year and relatives are putting pressure on them. However, her TB status cannot be revealed to their relatives. The husband also shares that because of TB their neighbours have stopped visiting their home.
As a Counsellor/NTEP staff you counselled her on the importance of adherence, hygiene and caregiver counselling along with stigma, discrimination and the importance of protection during physical relationships in this period.
Today Jayanti has come with her husband and mother-in-law and she shares that she is two months pregnant as she could not bear the remarks by the family. Jayanti’s husband is really concerned about Jayanti because she has left medicines as she wants to continue with the pregnancy. No one in her family has forced her but she herself feels that there is no harm if she continues with the pregnancy. She says she can continue the treatment after the delivery.
Please counsel her for restarting the treatment and the consequences of leaving the treatment incomplete. Clear her misconceptions and facilitate her to make the correct choices with appropriate referral, if required.
* Alternative:
Facilitator should first ask the participants in a plenary to brainstorm what are the problems that patients come up with when they are on TB treatment. When participants go on listing such problems, the Facilitator will register in mind who is sharing which problem and write each problem on the board. Then Facilitator will divide the participants in 3 to 5 groups, depending on the size of the batch. Once groups are formed, the Facilitator will assign one problem to each group to prepare and present the role play concerning that issue. Facilitator will ensure that each group has at least one member who had contributed to the list of problems before forming the groups. If not, will swap any of the participants from another group having more than one contributor. Thus, they will prepare and present the role play based on the same issue contributed by their group member. All the groups will be instructed to observe the role play of the previous group, monitor the time i.e. 5 minutes and give feedback-based Counselling soft skills used by the Counsellor in the roleplay, principles followed or not followed and anything that was found to be missing as long as counselling is concerned. After every role play and feedback by the next group, the Facilitator will conclude by focusing on the missing points or fallacies in Counselling.
Critical Issues in
Adherence
Counselling


Session Overview

Activity 1 : Brainstorming barriers to treatment adherence
Activity 2: In search of Solution
Summarisation
Master Trainer required for this session: TB Champions/ Some previous
experience in HIV /TB Counselling will be required.
Session Objectives

By the end of this session, participants will be able to:
Identify critical issues in adherence counselling.
Describe strategies to address psycho-social challenges in adherence to treatment.
Enlist appropriate steps and referrals required.
Time allowed
1 hour 15 minutes
Material required

- IJ Whiteboard and markers (or blackboard and chalk)
- IJ Chits of the statements from Annexure l for Activity 2- In Search of Solution
Method
Activity on the next page

Brainstorming Barriers to Treatment Adherence

You as a Facilitator will –
Ask all the participants the meaning of word adherence? Let 4-5 participants share their definitions or understanding of the word with the rest.
Next, ask everyone to stand up.
Ask – Now, only those who have never ever fallen ill in their life, till date can sit down.
Say- Now, only those who have never visited a doctor despite of being ill can sit down.
After this say – Now, only those who were not prescribed a course of antibiotics by the doctor can sit down.
Lastly, say – Now, only those who have completed all dosages of medicines and have never ever missed a single dose of medicine, ever in their life can sit down. At the end of this exercise majority of the participant will be standing.
Facilitator will highlight that, “In this group, despite being educated and urban, we were also not able to complete all the dosages of medicines every time. Thus, before we start this session, we need to be sensitive about the challenges of adherence, especially in continuing the treatment.
After this, Facilitators will ask the participants to brainstorm the list of reasons for non-adherence to treatment by saying, “Now, think about a person with TB and who is on treatment. What are the common reasons for non-adherence to the treatment? Ask them not to repeat any response. Facilitators will write the responses on whiteboard.
Finally, orient participants with the definition given by WHO as follows:
Adherence: “Extent to which a person’s behaviour; the taking of medication and the following of a healthy lifestyle including a healthy diet and other activities – corresponds with the agreed recommendations of the health care providers” (WHO, 2003)

Brainstorming Barriers to Treatment Adherence

This activity is based on Carousel, also called Margolis Wheel.
As a Facilitator you will –
Ask the participants to stand in a bigger circle, holding hands.
Then cut the circle in half and ask the participants to form two circles still holding hands. Name them Circle A and Circle B. (Refer to the picture in the Annexure 2). To avoid any disturbance while demonstrating the forming of concentric circles, Facilitator can order Circle A or B or both the circles to ‘freeze and release’, as per requirement.
Facilitator will demonstrate further division of Circle A into an inner and an outer circle by asking every alternate participant to let go of hands and by stepping one step inside the circle.
The participants in the inner circle will be asked to turn outside and adjust themselves in such a manner that each from the inner circle will face one participant from the outer circle.
The process will be repeated for the Circle B, in the same manner. This way two concentric circles will be formed. Ensure that the number of participants in both groups are even so that they can form pairs. If not, add or subtract.
Facilitators will instruct all the participants that those who are in the inner circle will play the role of the DR-TB Counsellors/NTEP staff. Those in the outer will be Patients who are taking TB treatment.
Each participant in the outer circle will be given a chit (See the Annexure l) with a specific problem statement related to TB treatment adherence which will be stated/voiced by them when the exercise begins. They will be asked to read their problem, understand it well before starting the activity.
Facilitator needs to instruct the participants in the outer circle that they have to discuss the same problem with all the counsellors in the inner circle, one by one.
When the Facilitator blows the whistle to start the exercise, the Counsellors will be stationary and not move, while the Patients will seek advice on their problems from the Counsellor.
The Patients will have 3 minutes with each Counsellor and at the sound of the whistle they will move clockwise from one Counsellor to the next.
Each pair of Counsellor and Patient will get only 3 minutes to discuss the case where Patient will share the problem with the Counsellor and Counsellor is supposed to listen to the problem and then provide counselling to the client. After 3 minutes, the whistle will be blown by the Facilitator and the Patient will move clockwise to the next Counsellor with the same problem. Note that the Facilitator will blow whistle after 3 minutes only for the first interaction between Counsellor and the Patient. But for subsequent interactions Facilitator will go on reducing the time by 15 to 30 seconds. Thus, the time to finish counselling with the last Patient will be l minute or less.
The movements can be stopped once the Patient meets all the counsellors in the outer circle. Facilitators will ask all the participants to get back to their seats and share their experiences of this counselling process. Facilitators will invite 2-3 participants from each group to volunteer to discuss their experiences. The Facilitators can make their own list of questions, but following are some examples that can be asked to both groups:
Counsellors’ volunteer – Were you able to listen to the problem properly? How did you solve the problem? What was the response of the Patient to the solution?
Facilitators will conclude this activity by indicating how the same problem can be addressed by different Counsellors differently, or how the same solution is accepted or is feasible depending upon the skills used by different Counsellors. Facilitators can highlight the limited time allotted to them.
Facilitator will then disclose the secret that the counsellors were not given 3 minutes for all Patients. In fact, they were given only l minute for the last few Patients and still they could counsel in one minute. Thus, Counselling is possible in one minute, as well. For this, counsellor has to assess the need of the Patient and provide need-based counselling, using soft skills.
Facilitator should also remind all participants that in reality, many of them will get such limited time for adherence counselling in the centre. Counsellors need to manage their time in such a manner that the saved time can be best utilized for the Patients who need more than average time. Hence, this activity provides them with a hands-on practice of their counselling skills.
Important to note that Counselling does not need a separate place or a lot of time. Counselling can happen in crowded spaces and limited time. However, audio-visual privacy has to be ensured.
Summarisation
Facilitators will summarise the session by focusing on the following key points.

Key points:
TB Patients are likely to face various challenges while undergoing TB treatment. As was discussed in the first session, a large number of these issues could be psycho – social such as poverty, stigma (actual or perceived), discrimination, Gender, substance abuse, mental illness, unemployment, lack of knowledge, etc. There could be more reasons such as occupational hazards, reproductive health, societal seclusion (single person living alone-Orphan, old age), medical issues with ADR, service providers’ behaviour which are also responsible for adherence. It is important to begin by identifying the challenges/needs, prioritising them and develop strategies along with the Patients to address the challenges.
Counselling should be Patient-centric.
Counselling is possible in shorter period and also in an unstructured set up. Patients need to be involved in the solutions; decisions should not be unilaterally taken on their behalf.
Adherence to treatment will not be possible unless we address psycho-social
challenges of TB.
Questions on Critical Issues in Adherence Counselling

1) A woman aged 27 years, recently married, was diagnosed with TB and started treatment. Identify the aspects a
Counsellor needs to address, while counselling this TB Patient for treatment adherence.
i. Counsel the TB Patient, TB Patient’s husband and other household members on the importance of successful treatment completion.
ii. Counsel the TB Patient’s husband and other household members on any stigma/discrimination towards the Patient.
iii. If required, link the TB Patient to the appropriate nutrition support service.
iv. All of the above.
2) A man aged 25 years who is a migrant labourer was diagnosed with TB and started treatment. While counselling this TB Patient, it is important to:
i. Counsel on cough hygiene and sputum disposal
ii. Counsel on availability of free TB treatment at his nearest government health centres and importance of adherence to treatment even if he migrates again.
iii. Counsel the family caregivers of the Patient, as they are staying away from him.
Annexurel
Note: Make minimum of two sets of the following statements
My cough is better, I am feeling much better, I need not take medicines any more ….
I leave early to my fields so I forget to take medicines….
I am scared to come to the PHC/DTC to take medicines as someone will see me…
I stopped medicines as I have a lot of headache and vomiting …
I am fed-up with prolonged treatment. So, I want to stop the treatment…
I think, even if I stop my treatment for some time, there is no problem…
I avoid coming to the centre as I am scared that somebody will see me…
I have shifted to a new house elsewhere. This centre is too far for me to pick up the medicines regularly…
Link for Hindi translation for case studies for Critical Issues in Adherence Counselling
https://drive.google.com/drive/folders/1X0fYkp7wfQVDyN4tE3C_7N7EPCHVP1ci
Annexure2
Annexure2
![]()
![]() Process of forming two concentric circles in Activity 2- Adherence Counselling: In Search of Solutions
Process of forming two concentric circles in Activity 2- Adherence Counselling: In Search of Solutions



Our words … Our Perspectives
Hamare Shabd … Hamara Nazariya
Our words … Our Perspectives
Hamare Shabd … Hamara Nazariya


Session Highlights

Session overview
Activity l -Self-introspection exercise- Hamare Shabd…. Hamara Nazariya…
Conclusion and key messages
Session Overview

Words are the vehicle of Counselling. Since, the words that we use can be so powerful, it is important to choose our words carefully while Counselling Patients. Words can convey love, hope, strength, truth, balance and compassion, or they can convey doubt, fear, distrust, confusion and discouragement. Certain words or phrases commonly used by us can undermine the effectiveness of the Counselling process, conveying unintended meanings and causing resistance to Counselling. Plenty of obvious words fit this category, such as name-calling, shaming words and words of defeat. In this session, we are going to see some such examples.
Session Objectives

By the end of this session, participants will be able to:
Understand what are the words and phrases that may be harmful to Counselling.
Understand what are alternative words which are less harmful to Counselling.
Give more insight about using appropriate language and thus sensitise Counsellors/ NTEP staff to become non-judgemental and all-inclusive.
Make them empathetic towards Patients.
Time allowed
30 minutes
Material required

- IJ Annexure l with statements for the Facilitator to read aloud
Method

Self-introspection Exercise – Hamare Shabd…. Hamara Nazariya…

You as a facilitator will-
Ask all participants to gather at the centre of the hall and stand in a circle but facing outside the circle. Ask all the participants to stretch out their right hand and ensure there is enough distance, so they do not touch one another. (Refer to Picture in Annexure)
Stand in the centre of the circle and instruct the participants to raise their right hand if they want to change the statements that would be read out by the Facilitators. If they don’t want to change the statement or are not sure, they should not raise their hand.
Then instruct all participants to keep their eyes closed throughout this activity. Participants are not supposed to speak anything during activity.
Next, read out the statements from the annexure, one by one. The tone of the Facilitators while reading these statements should not be neutral but offensive, provocative, biased, casual, emotional, as per the content of the statement to convey how the general remark made by the staff will sound.
Before moving to the next statement, Facilitator has to say – ‘hands down’, even if no one has raised a hand.
Conclude this activity by saying that even though we all are not sure of the correctness of our response to some of the statements, the main purpose of the activity was self-introspection and to move towards changing our perspectives towards Patients.
At this point, Facilitator will write 3 A’s on the board – Aware, Accept and Action and explain them one by one. Becoming ‘Aware’ of one’s own attitudes and perspectives. Then if the attitude or perspective is wrong in any way, ‘Accept’ it as wrong. Lastly, if the perspective or attitude was wrong then the third ‘A’ is the need to take ‘Action’ to change it. On this note, Facilitator will say that through this training we can only take them to the first ‘A’ i.e. Awareness. But the next two ‘A’s – i.e. ‘Accept’ and ‘Action’ are to be taken by each one of them on their own.
Note for the Facilitators

To have an impact of the activity, complete silence and seriousness are to be maintained during this activity. Hence, there will be absolutely no discussion or whispering with Co-Facilitators or any of the participants which might divert everyone’s attention.
Ensure that all participants have closed their eyes before starting the activity.
Facilitators should read out each statement with an appropriate emotional tone – such as rudeness, anger, casual approach, too friendly, etc. – suitable to the content. Facilitator should practice these statements in advance and should read them aloud in an audible pitch. These statements can be repeated, if needed.
After each statement, Facilitator will look at the participants’ response and ask them to put their hands down, even if none of the participants has raised their hand for any of the statements.
Conclusion

Then Facilitator will conclude the session by focusing on following key points-
Key points for emphasis:
Our language conveys our attitudes. As a Counsellor/NTEP staff, it is important for us to be aware of our language and use it appropriately.
As NTEP staff, we also need to understand that this person is a Patient during this specific situation or moment, and that is not their identity.
Patients can be men, women and TG and we should use inclusive pronouns like “they” instead of using only “he”.
Annexure
Statements
For Our words…. Our perspectives (Hamare shabd Hamara Nazariya)
➔ Patients are illiterate. They don’t understand medicines.
➔ Why are you worried/tense? So many people have TB, it is not a big deal.
➔ I am like your brother/sister/son/daughter, you will take medicines for me na?
➔ This is not my work.
➔ If you die, who will look after your children?
➔ This Patient is an alcoholic; he won’t take the medication.

Activity: Self-introspection exercise: Our words Our Perspectives
Link for Hindi translation of statements for Our Words Our Perspectives
https://drive.google.com/drive/folders/1csLHoYRM9J-N-PB1HDGxK_Vynsqyh7PY
Going Ahead Hum Hain Saksham
Going Ahead…
Hum Hain Saksham



Session Overview

Activity 1 : Going ahead ….Hum Hai Saksham
Activity 2 : Vision Board – Hamari Manzi/
Master Trainer required for this session: CBC/STDC staff/Any MT
Session Objectives

By the end of this session participants will be able to:
Get known to one’s own strengths and capabilities.
Create a road map and motivate themselves to achieve their goals.
Time allowed
l hour 15 minutes
Material required

IJ Chart papers
IJ A4 size coloured papers
IJ Crayons
IJ Sketch pens
IJ Scales, scissors, glue, pencils, erasers, sharpeners
IJ Craft and decorative material – glitter, ribbons, beads
Method
You as a Facilitator will –
Inform the participants that this is the last session of the training.
Congratulate them on being receptive to learning and growth.
Inform them that we are now going to undertake two activities to set the tone for how they would resume their work and get motivated to do so.

Going Ahead ….
Hum Hai Saksham

Ask all the participants in a plenary to share two things they learned during the training that they will immediately start using, or make some changes in the way they perform their duties. Also, ask each one of them to appreciate one of the participants and share the reason for their appreciation by reporting a particular quality they liked about that person. (Facilitator can use a smiley or a teddy bear for this activity to use as a token of appreciation).
Ensure that each participant shares – it can be any of the micro-skills, principles of counselling, change in attitude, quality of effective counselling, things that they would avoid while counselling, information related to social protection linkages, or gender.
Appreciate the participants for their responses and for also for actively participating during the training.
Remind them that they have all the knowledge and skills for them to achieve NTEP goals. They are “Saksham “, “Truly Saksham”, “Sachmuch Saksham”!!

Vision Board – Hamari Manzi#

Ask the participants in the plenary if they have any experience in life where their wish was surprisingly fulfilled. Request one or two participants to share their real life experiences in short. Conclude this by talking about the power of wishful thinking or affirmations in life.
Ask them if anyone knows about vision board and if has anyone used it in their personal life to fulfil their dreams.
If any, ask that participant to speak about that vision board. Emphasise that the vision board must have and specific demand and exact time/date/year mentioned along with it to have the expected results/ achieve the goal.
Now ask participants what is the goal or target of NTEP? What is the timeline? Then introduce the theme of the vision board that they are going to make in a creative manner by saying – “We all are aware and committed to End TB by 2025. Now let us develop a vision board. A vision board is a collage of images and notings, designed to serve as a source of aspirations and motivations (See the picture in the Appendix) to help us achieve this goal. Please write the steps of exactly how you want to do this… e.g., reduction in LFU, reduction in number of deaths, using appropriate attitudes, following principles and counselling skills etc. The topic of the vision board is – ‘End TB by 2025’.”
For this, divide the participants into 2 or 4 groups, depending on the number of participants. If there are staff from the same OTC, put them in the same group.
Give each group a chart paper, colourful sketch pens and decorative material. Ask the groups to decorate the chart paper. Allow 30 minutes ohime for this. After completion, ask groups to display their chart papers.
Conclusion
Participants can carry their vision board with them or make similar vision boards when they go back to their OTO with their other colleagues and display it in the OTC. Alternatively, the vision boards can also be displayed in the STOC.
This will provide a road map and motivate them to achieve their goals.
Wish participants the best and assure them that “Together we will end TB by 2025.”
Play the TB anthem and form a chain and dance together. (See the picture in the annexure) (TB Harega Desh Jitega song link – https://www.youtube.com/watch?v=R-Oz4Fc6g74)
Lastly, stand in the circle and say aloud together twice- ‘TBHarega, Desh Jitega’ – with thumbs-down sign for TB Harega and thumbs-up sign for Desh Jitega. (If participants are multilingual, have this slogan in different languages for such participants, to have unity in diversity).
Lastly, conclude by saying that this is the wish that we are sending to the Universe and that the Power in the Universe will definitely help us achieve it by 2025!!! Everyone clap together.
Ensure that this activity is a lot of fun for the participants and they feel energized and motivated. You can play motivational songs in the background while this activity is being conducted.
Annexure
Picture of a Vision Board for representation purpose


Forming a chain and dancing together on TB anthem – TB Harega Desh :Jitega
song at DR- TB Counsellors Training, Mumbai
Energiser
Energiser
![]()
![]() Signature
Signature
Time: 5 Minutes
Objective: To make the participants alert and active
Method:
Ask all the Participants to stand in a circle keeping some distance from each other. Facilitator will demonstrate and ask the participants to follow these steps:
Request the participants to try writing their names in the air with their right hand.
Next with their left hand.
Then with the right foot by lifting it a little. Now with the left foot.
Now while standing straight and resting their hands on their waist, tell them to try writing it with the waist movements.
Tips for Resource person/Trainer: The Facilitator too should be part of the group and do all the actions, thus encourage all to participate.
Jungle Mein Aag Lagi… Bhago… Bhago… Bhago…(The Mountain is on Fire… Run! Run!! Run!!!)
Time: 5 Minutes
Objective: To make the participants alert and active, can also be used for dividing participants in smaller groups for various activities
Method:
Ask all the Participants to stand in a circle keeping some distance from each other.
Facilitator will explain the activity by saying that – Now I will say aloud- Jungle Mein Aag Lagi Bhago… Bhago… Bhago… {The Mountain is on Fire… Run! Run!! Run!!!) and run in the same direction in a circle. I will increase or decrease the speed and volume of my speech and you will have to adjust your volume and speed, accordingly. In between, I will utter a number aloud. Immediately, you will have to make groups with that number of participants in it. Remember, the group size has to be of the same number- not more or not less. If anyone is not able to find the partner to form a group that person can run anywhere and find partners to form a group of the said number.
Facilitator should go on announcing the numbers randomly and at the end say the number that the Facilitator wants to form the groups into for the activity that will follow.
Tips for the Resource person/Trainer: The Facilitator should also stand inside the circle and encourage all the participants, by running in the same direction but inside the circle, keep changing the pitch of the voice. If anyone who is not willing to run or cannot run due to age or physical handicap/ illness can be allowed to sit aside and not be part of this activity.
Fruit Salad
Time: 5 Minutes
Objective: To make the participants have fun and exercise
Method:
➔ Ask all participants to stand in a circle keeping some distance from each other.
➔ Facilitator should stand at the centre of the circle and ask everyone to imitate the Facilitator.
➔ Facilitator will sing an action song- which includes both singing and acting according to the words of the song.
➔ The words of the song are Watermelon,Watermelon, Papaya, Papaya, Cheekoo,Cheekoo,Cheekoo Cheekoo,Cheekoo,Cheekoo Fruit Salad, Fruit Salad.
➔ This could be sung using the tune of the nursery rhyme- ‘I hear thunder’. The Facilitator can use any other tune that would be peppy and interesting.
➔ While singing the Facilitator will also act. While singing ‘Watermelon’ they will make big circle in the air with their hands, starting from top and bending down to complete the circle to indicate a large watermelon. Then make a shape of a
big Papaya, then lift the right hand upwards and show the shape of a small Cheekoo by twirling their fingers in circular fashion while saying Cheekoo…Cheekoo…Cheekoo…for the first time and then should do the same action with other hand while singing Cheekoo…Cheekoo…Cheekoo….for the second time. Finally, the Facilitator will say Fruit salad and while saying so twirl around themself with hands slightly extended.
➔ All the participants will repeat every line of the song and the action after the Facilitator.
➔ The Facilitator will bring more fun into activity by changing the tempo of the song and the speed of action. They may begin slowly and gradually increase or decrease the tempo. The activity can have 2-3 rounds.
Tips for Resource person/Trainer: The Facilitator should also stand inside the circle and demonstrate all the actions, thus encourage all to participate. Faci Iitator shou Id ensure that this activity is be joyfuI.
Link for some more energisers:
https://drive.google.com/drive/folders/1QBChzy6HsAvXAhuEczhQqA0O0R_s9juD
Thank you!

Published and disseminated by: Saksham Pravaah,
Tata Institute of Social Sciences,
V. N. Purav Marg, Deonar, Mumbai-400088, India
Office: 91-22-25525491 I Email: saksham@tiss.edu
Website: www.tiss.edu
Design by



